Navigating “what are the latest treatments for atrial fibrillation”? The newest procedures, including Pulsed Field Ablation, and the evolution of genetically tailored anticoagulants are setting the stage for a new era in AFib care. This concise guide sheds light on such innovative therapies, designed to enhance patient outcomes without wading through the complexities of medical terminologies.
Key Takeaways
- New advancements in AFib treatment, like Pulsed Field Ablation (PFA) and Left Atrial Appendage Closure (LAAC), focus on specific targeting, efficiency, and stroke prevention, representing significant improvements in managing the condition.
- Catheter ablation, supported by advanced mapping and ablation technologies, is a key treatment option for AFib, with its efficacy dependent on careful patient selection and consideration of individual health statuses.
- Personalized medicine is essential in AFib management, which involves tailoring treatment and medication plans based on individual genetic factors, lifestyle, and other health conditions to ensure optimal patient outcomes.
Emerging Therapies in Atrial Fibrillation Management
Atrial fibrillation, an irregular heart rhythm in the upper chambers of the heart, can lead to inefficient blood pumping, complicating the patient’s life with symptoms ranging from heart palpitations to chest pain. This irregular heartbeat, also known as atrial fibrillation, has primary goals of management that include resetting and controlling the heartbeat and preventing the formation of blood clots that could lead to strokes.
In the pursuit of improved health outcomes, the advent of new treatments like Pulsed Field Ablation (PFA), Left Atrial Appendage Closure (LAAC), and novel anticoagulants offers renewed hope and creates a wide range of possibilities for effective management of this condition.
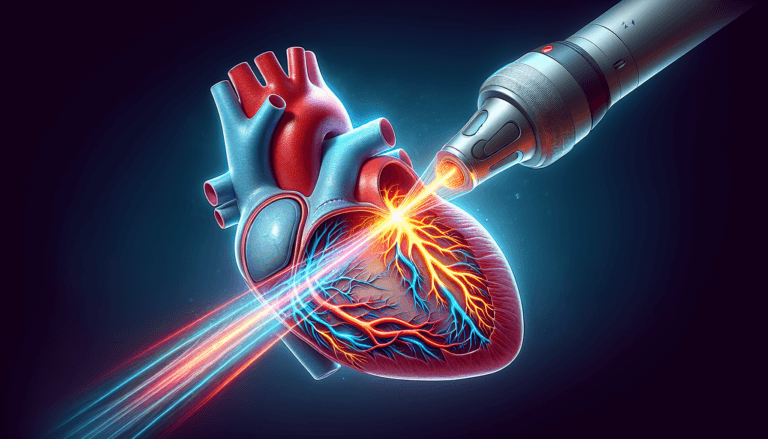
Pulsed Field Ablation (PFA)
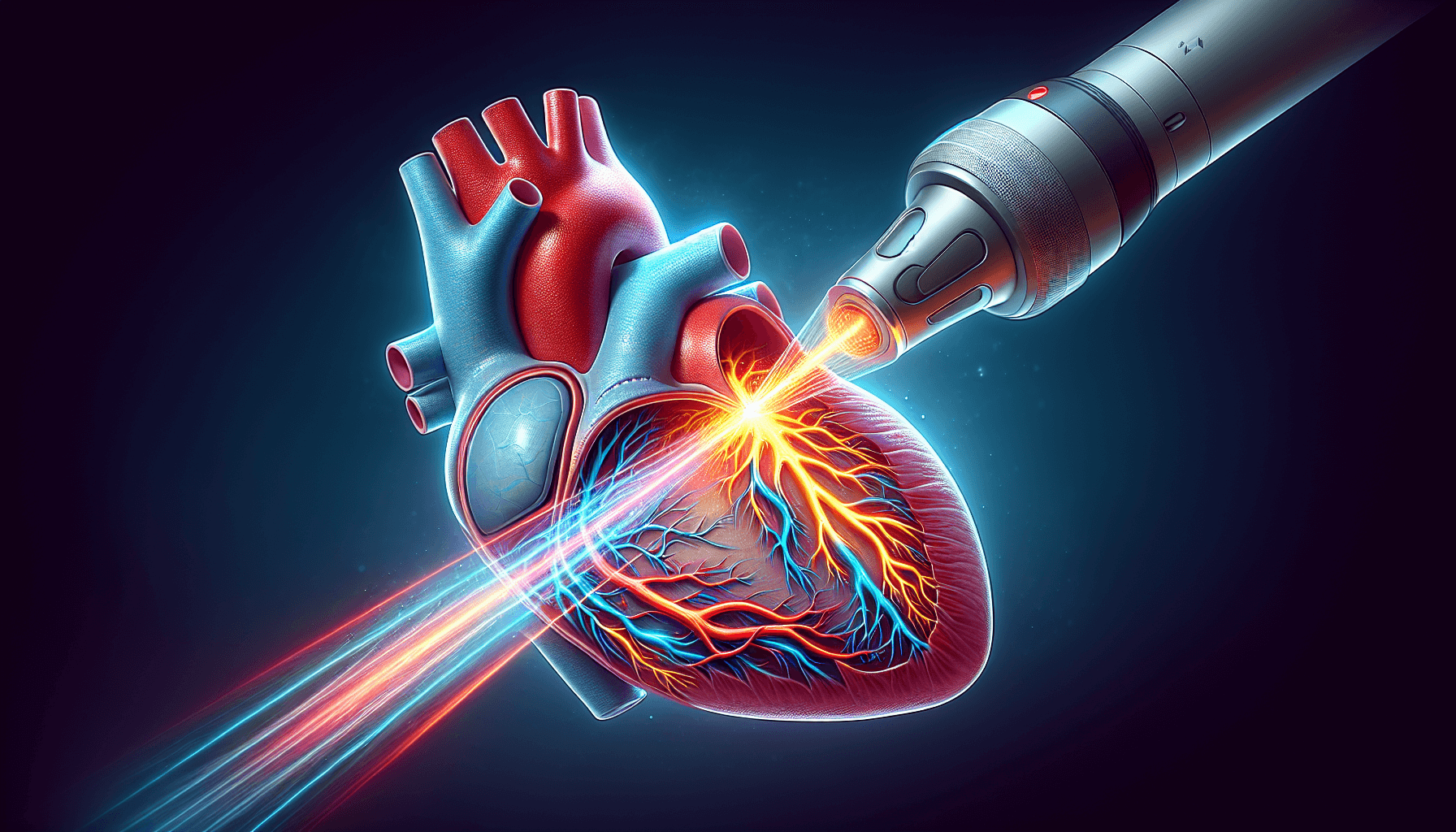
Pulsed Field Ablation (PFA) is a revolutionary new technology that uses controlled electric fields to specifically target and treat heart tissue causing recurrent paroxysmal atrial fibrillation (AFib). This procedure stands out for its specificity, safety, and efficiency, holding significant promise in AFib treatment. One of its potential advantages over traditional thermal (also known as burning energy) ablation methods is that it creates precise myocardial lesions without heating nearby tissue, thereby minimizing the risk of damage to adjacent structures such as the esophagus and nerves.
Additionally, the efficiency of PFA procedures is showcased by the significantly reduced operation time, with many procedures completed in under an hour. This efficiency has led to significant improvements in patient quality of life with a very low adverse event rate. As a cutting-edge procedure with promising results in clinical development, PFA has the potential to reduce the incidence of complications like pulmonary vein stenosis, making it a compelling option for AFib treatment.
Pulsed Field Ablation (PFA) Clinical Trials and Data
Clinical trials have been instrumental in evaluating the efficacy and safety of Pulsed Field Ablation (PFA). One such trial is the FARAPULSE PFA (Adaptive Contact) Study, which demonstrated a 75% success rate in maintaining sinus rhythm at 12 months post-procedure in patients with paroxysmal atrial fibrillation. This trial included a cohort of 121 patients and reported a significant reduction in AFib episodes without the need for further anti-arrhythmic drugs.
Another pivotal study is the PULSED AF pivotal trial, which showed that PFA had a 12-month freedom from atrial arrhythmias rate of 80.4% in treated patients. This trial’s safety outcomes were equally promising, with a very low incidence of procedure-related serious adverse events.
The PFA-5 Trial, a multicenter study, reported an 85% success rate of PFA in isolating pulmonary veins with a single application of the PFA technology. Safety data from this trial highlighted the absence of esophageal or phrenic nerve injury, underscoring the procedure’s safety profile.
These trials indicate that PFA is not only effective in achieving pulmonary vein isolation and reducing AFib recurrence but also maintains a high safety standard, with minimal risk of collateral damage to adjacent tissues, which is a common concern with thermal ablation techniques.
FDA Approval of Pulse Field Ablation Systems
The medical community has welcomed the recent FDA approval of Pulse Field Ablation (PFA) systems developed by leading companies such as Medtronic and Boston Scientific. These approvals mark significant milestones in the field of cardiac electrophysiology. Medtronic’s PulseSelect PFA system, which received FDA approval in December 2023, offers a unique approach to treating atrial fibrillation by delivering pulsed electric fields to ablate heart tissue selectively without affecting surrounding structures. Boston Scientific’s FARAPULSE PFA system, also granted approval in January 2024, features advanced algorithms and catheter precision, providing physicians with an innovative tool to treat patients with AFib more safely and effectively. The sanctioning of these systems is expected to revolutionize the management of atrial fibrillation, offering a new standard of care with potentially fewer complications and shorter recovery times.
Left Atrial Appendage Closure (LAAC)
The Left atrial appendage closure (LAAC) procedure presents another significant advancement in AFib management. It works by sealing off the left atrial appendage, where blood clots are most likely to form, thereby preventing strokes in patients with atrial fibrillation. The WATCHMAN device is one of the LAAC technologies that has become a significant focus for integration into clinical treatment for AF patients at risk of stroke.
Ongoing clinical trials, including those spearheaded by the Mayo Clinic, are thoroughly investigating the safety of the WATCHMAN device. This is a vital step towards its approval and use in managing heart health. The LAAC procedure, therefore, holds immense potential for stroke prevention in AFib patients, improving their quality of life and reducing stroke risks.
Advancements in Traditional Radiofrequency Ablation Equipment
The field of traditional radiofrequency (burning energy) catheter ablation has also seen significant advancements the last several years with the introduction of high definition mapping catheters and the adoption of high power short duration (HPSD) catheters. These innovations are designed to improve the efficacy and safety of radiofrequency catheter ablation for the treatment of atrial fibrillation and other arrhythmias.
High definition mapping catheters are a leap forward in the precision of cardiac mapping. They utilize a dense array of electrodes that can capture a high volume of data points from the heart’s electrical activity. This allows for a more detailed and accurate visualization of the cardiac anatomy and the arrhythmogenic substrate. The enhanced resolution provided by these catheters facilitates the identification of critical arrhythmia circuits and focal points, enabling more targeted and effective ablation.
The adoption of HPSD catheters represents another major stride in ablation technology. These catheters deliver higher power energy for a shorter duration to the targeted tissue, which has been shown to create more durable lesions with a reduced risk of collateral damage. The HPSD approach allows for a more efficient transfer of energy, leading to a decrease in the overall procedure time and potentially improving patient outcomes.
By combining high definition mapping with HPSD catheters, electrophysiologists can achieve a greater level of control and precision during ablation procedures. This synergy enhances the likelihood of successful pulmonary vein isolation and reduces the chances of arrhythmia recurrence, which is a common challenge in AFib management.
These technological advancements in traditional radiofrequency ablation equipment are pivotal in refining current treatment protocols and offer patients with cardiac arrhythmias a more effective therapeutic option.
Novel Anticoagulants
The introduction of novel anticoagulants represents another important stride in AFib management. These medications are being designed to account for genetic variability in patients, which can influence the effectiveness of drug therapy for atrial fibrillation.
This personalized approach to anticoagulant therapy, including the use of blood thinners, allows for more accurate and effective treatment, reducing the risk of stroke and improving patient outcomes.
New Blood Thinner Clinical Trials: Abelacimab for Atrial Fibrillation
One of the most promising clinical trials in the realm of anticoagulants for atrial fibrillation is focused on the newest blood thinner, abelacimab. Abelacimab represents a novel class of anticoagulants that targets Factor XI, a clotting factor involved in the intrinsic pathway of the coagulation cascade. By inhibiting this factor, abelacimab aims to reduce the risk of thrombosis without significantly increasing the risk of bleeding, which is a common side effect of many anticoagulants.
The clinical trial for abelacimab is designed to assess its efficacy and safety in comparison to traditional anticoagulants like warfarin and the newer direct oral anticoagulants (DOACs). This trial involves patients with non-valvular atrial fibrillation who are at an elevated risk for stroke. The primary outcome measures include the incidence of stroke, systemic embolism, and major bleeding events.
The potential benefit of abelacimab lies in its dual-action mechanism, which not only prevents the formation of blood clots but also does so with a potentially lower risk of causing bleeding complications. This could be particularly beneficial for patients with atrial fibrillation who have a high risk of stroke but are also at risk of bleeding due to anticoagulation therapy.
If successful, abelacimab could revolutionize the management of atrial fibrillation, providing a safer and more effective anticoagulation option for patients. The results of this clinical trial are eagerly awaited by the medical community, as they may lead to a new standard of care for anticoagulation in atrial fibrillation patients.
The Role of Catheter Ablation in AFib Treatment
Catheter ablation represents a significant component of AFib treatment. This minimally invasive procedure uses radio frequency energy to treat irregular heartbeats, disrupting irregular heart signals and restoring a normal heartbeat. New guidelines even advise cardiologists to consider cardiac ablation as a first line of defense for patients with AFib, marking a significant shift in treatment approach.
The choice of surgical options such as catheter ablation over medicinal treatment for certain AFib patients may reduce AFib-related deaths. However, it’s important to note that patients with persistent AFib may experience a lower long-term success rate with ablation when compared to those with AFib of shorter duration.
Advancements in Technology
The technology supporting catheter ablation has seen substantial improvements in recent times. Devices like the Octaray Mapping Catheter with Trueref Technology, The HD Gird Mapping Catheter, and the Optrell Mapping Catheter with Trueref Technology represent significant advancements in the mapping of complex cardiac arrhythmias, supporting more precise treatments for atrial fibrillation.
Further advancements are seen in the Qdot Micro Catheter’s high-power, short duration, temperature-controlled ablation and Cryoablation’s freezing techniques, which both focus on creating effective lesions to block abnormal electrical impulses.
Electrode catheters have also evolved to offer more precise targeting and treatment of abnormal heart tissue, improving the safety and efficacy of ablation procedures for atrial fibrillation. I frequently tell my patients that the equipment used in catheter ablation improves every year, with new generation equipment and new features.
Patient Selection Criteria
While catheter ablation is a promising treatment option, the selection of patients for this procedure is crucial. The selection criteria include consideration of heart failure status, previous stroke or dementia events, and rates of death alongside having no structural heart issues and presenting symptoms from AFib. Conditions like left ventricular systolic dysfunction, obstructive sleep apnea, and atrial tissue fibrosis are also reviewed when assessing eligibility for catheter ablation, as they can influence the procedure’s success outcomes.
The complexity of atrial fibrillation and the overall burden of the condition are clinical predictors that are taken into account to evaluate the probability of a successful ablation procedure. However, it’s important to note that older patients and those with more complex heart conditions may face higher risks during catheter ablation and may benefit more from medication management rather than ablation procedures.
Addressing Risk Factors for Atrial Fibrillation
Managing atrial fibrillation is not only about the treatments and procedures but also about addressing lifestyle and risk factors. These include:
- Alcohol abuse
- Smoking
- Sleep apnea
- Obesity
These factors significantly impact the incidence of atrial fibrillation. In addition, lifestyle modifications improve the success rates of an ablation procedure for atrial fibrillation.
For early AFib management to prevent its progression, a heart-healthy lifestyle, including regular exercise and a healthy diet, is recommended.
Lifestyle Modifications
Significant improvement in AFib management can be achieved by addressing lifestyle factors. For instance, reducing or eliminating the consumption of caffeine and alcohol may alleviate symptoms of arrhythmia. Quitting smoking and the use of tobacco products is crucial for heart health, with programs available to assist individuals in cessation.
Furthermore, engaging in regular physical activity, like daily 30-minute brisk walks, can aid in weight loss, reduce high blood pressure, and decrease the likelihood of an AFib. In essence, adopting lifestyle changes such as eating healthy foods and exercising more is a key approach to control atrial arrhythmia recurrence.
Importance of Blood Pressure Control
In addition to lifestyle modifications, maintaining blood pressure within a healthy range is vital to prevent the progression of atrial fibrillation. High blood pressure is a key risk factor that needs to be controlled. Other comorbidities alongside blood pressure should be taken into account when managing atrial fibrillation.
A comprehensive risk evaluation including factors beyond the CHA2DS2-VASc scores influences the customization of anticoagulant therapy. Thus, blood pressure management is an integral part of the comprehensive assessment for the use of anticoagulants in patients with atrial fibrillation.
The Indispensable Role of Lifestyle Modifications in AFib Management
Despite the remarkable strides in technology for atrial fibrillation (AFib) ablation, it is important to recognize that these advancements do not replace the critical role of lifestyle modifications in the long-term management of AFib. While devices such as the PulseSelect Pulsed Field Ablation (PFA) system represent significant progress in the treatment of AFib, they work best when complemented by a patient’s commitment to a healthy lifestyle.
Lifestyle changes are the cornerstone of AFib management and can significantly reduce the frequency and severity of episodes. These modifications include maintaining a balanced diet, engaging in regular physical activity, managing stress, and avoiding known triggers such as excessive caffeine and alcohol intake. For many patients, weight management through diet and exercise can lead to a noticeable reduction in AFib symptoms.
Moreover, managing risk factors like hypertension, diabetes, and sleep apnea is essential in preventing the progression of AFib and its complications. Blood pressure control, in particular, can have a profound impact on the effectiveness of any ablation technology, as uncontrolled hypertension can lead to structural changes in the heart that may predispose individuals to arrhythmias.
In essence, while new ablation technologies offer exciting possibilities for the treatment of AFib, but they do not negate the necessity for patients to adopt and maintain healthier lifestyles. These lifestyle choices lay the foundation for any technological intervention to be effective and for patients to achieve the best possible outcomes in AFib management.
Personalized Medicine and AFib: Tailoring Treatment to the Patient
Within the sphere of AFib management, the importance of personalized medicine is increasingly being recognized. This involves tailoring treatment plans to individual patient characteristics, including genetic factors and customized anticoagulation therapy.
This approach guarantees that each patient receives a treatment plan that is most likely to be successful in managing their specific case of AFib.
Genetic Factors and AFib
Genetic variations in patients can lead to different responses to AFib medication, impacting the efficiency of treatment strategies. Rare genetic variants and common genetic polymorphisms associated with AFib can have significant implications for a patient’s therapy response.
Patients with AFib who carry certain genetic variants may respond differently to rate-control therapy, and these variants can influence the adequacy of ventricular rate control. Therefore, developing anticoagulation therapy plans for AFib patients can involve assessing genetic determinants that predict the effectiveness of rate control medications.
Providing a family health history, including conditions like heart disease and diabetes in close relatives, can also offer insights into potential health risks for the patient.
Customizing Anticoagulation Therapy
Customizing anticoagulation therapy involves a comprehensive stroke risk assessment, considering factors beyond the CHA2DS2-VASc score and examining other comorbidities and risks. The choice of anticoagulation therapy is influenced by additional patient-specific factors including age, concomitant drug use, renal function, and individual bleeding risk, which is evaluated using risk assessment schemes like HAS-BLED, ATRIA, and HEMORR2HAGES.
For instance, Warfarin dosage variability is often attributed to genetic factors that impact the drug’s metabolism and patient receptivity, which are considered when customizing anticoagulation therapy. Clinical trials, such as the Edoxaban versus Warfarin study, inform and refine anticoagulation treatment approaches, especially for patients with complex needs, like those who have undergone heart valve replacement procedures.
For atrial fibrillation patients at high risk of bleeding, left atrial appendage closure has emerged as a class 2a recommendation, providing an alternative to long-term anticoagulation therapy.
Clinical Trials Shaping the Future of AFib Treatment
The future of AFib treatment is being shaped by ongoing clinical trials. These trials are evaluating new interventions and technologies, such as PFA, nMARQ Catheter System, and AI for stroke prevention. The results from these trials contribute to the development of new treatment options, leading to regulatory approval and the introduction of new standard care for patients with atrial fibrillation.
Participating in Research
By participating in clinical trials, patients can actively contribute to the advancement of personalized medicine to treat atrial fibrillation. Clinical trials comparing different therapies, such as percutaneous left atrial catheter ablation versus anti-arrhythmic drug therapy, are conducted to establish which approach is more effective in reducing mortality, stroke, bleeding, or cardiac arrest in atrial fibrillation patients.
Studies are also conducted to establish the safety and effectiveness of devices like the WATCHMAN Left Atrial Appendage Closure Device for patients with non-valvular atrial fibrillation who are ineligible for anticoagulation therapy. Clinical trials often examine the use of novel medications, such as edoxaban compared to traditional vitamin K antagonists, in patients who have undergone heart valve replacement via catheter and have atrial fibrillation.
Some trials, like the ORBIT-AF II registry, collect observational data to evaluate the outcomes related to the use of new antithrombotic agents in broad patient populations outside of clinical trials.
From Trial to Treatment
The transition from clinical trials to standard treatment is a critical phase in the advancement of AFib management. The results from clinical trials can lead to the approval of new treatments when significant evidence is found.
For example, early clinical trials of PFA have shown effective and safe pulmonary vein isolation, leading to its commercial approval in January 2021. Studies such as the comparison of dual therapy with dabigatran versus triple therapy with warfarin are crucial in establishing evidence that may result in new treatment guidelines for AFib patients undergoing percutaneous coronary intervention.
Navigating Healthcare: Collaborating with Your Cardiologist
A collaborative approach with a cardiologist is fundamental to the effective management of AFib. This involves preparing for appointments, understanding treatment plans, and maintaining open communication about medical history and symptoms.
The primary care doctor plays a crucial role in overseeing the patient’s overall health, coordinating care with the cardiologist and managing other conditions that may coexist with AFib.
Preparing for Your Appointment
Several steps should be taken in preparation for a cardiologist appointment. Patients are advised to:
- Be aware of pre-appointment restrictions
- Document symptoms and personal information
- List medications and supplements taken
- Prepare questions for their cardiologist ahead of an AFib treatment appointment
Bringing a list of current medications, including names, dosages, and usage frequency, to the cardiologist appointment is essential for accurate medical records.
Having copies of recent lab results and tests from other healthcare providers can prevent the need for duplicate testing. Keeping an organized folder with all personal health information ensures easy access during healthcare visits.
Learning about one’s condition prior to the appointment allows for more productive discussions with the cardiologist. Writing down questions about the condition and prioritizing top concerns ensures important topics are discussed during the cardiologist visit.
Understanding Your Treatment Plan
To fully comprehend an AFib treatment plan, one needs to be familiar with the range of medications and procedural options available, and appreciate the significance of lifestyle modifications and routine health checkups. Patients should consult with their doctors before taking over-the-counter medications or herbal treatments as these may trigger arrhythmias.
Adherence to the AFib treatment plan is essential for managing the condition. This includes:
- Understanding the roles of various medications
- Understanding procedural options such as cardioversion and ablation
- Making lifestyle changes
- Regular health checkups
By following these steps, you can effectively manage your AFib and improve your overall health.
Summary
The landscape of AFib management is rapidly evolving, with new treatments, personalized medicine, and clinical trials promising better outcomes for patients. Lifestyle modifications and risk factor management play a significant role, and collaboration with a cardiologist is crucial for effective management. With advancements in technology and the emergence of novel treatments, the future is brighter for those living with atrial fibrillation. Together, patients, healthcare providers, and researchers can make strides in AFib treatment, improving the quality of life for countless individuals living with this condition.
Frequently Asked Questions
What is the most successful treatment for AFib?
Atrial fibrillation ablation is the most successful treatment option for patients who have failed or not tolerated medications. Other effective treatments include blood thinners to lower the risk of complications and heart rate-controlling medications such as beta-blockers.
What is the first drug of choice for atrial fibrillation?
The first drug of choice for atrial fibrillation is typically a beta blocker or a calcium channel blocker, such as bisoprolol, atenolol, verapamil, or diltiazem, depending on your symptoms and general health. If these are not suitable, digoxin may be offered as an alternative. Amiodarone, flecainide, propafenone, and sotalol are also options to consider based on the patient’s condition.
What is the permanent cure for AFib?
Unfortunately, there is no permanent cure for persistent atrial fibrillation. However, treatment and lifestyle changes can help manage symptoms and reduce complications effectively.
What is the newest treatment for atrial fibrillation?
The newest treatment for atrial fibrillation is the PulseSelect Pulsed Field Ablation (PFA) system, which gained FDA approval in December 2023.
What is Pulsed Field Ablation (PFA) and how does it work?
Pulsed Field Ablation (PFA) is a non-thermal ablation technology that uses controlled electric fields to specifically target and treat heart tissue causing recurrent paroxysmal atrial fibrillation (AFib). It creates precise myocardial lesions without heating tissue, minimizing the risk of damage to adjacent structures.
The Best Atrial Fibrillation Book
Your Complete Guide To AFib: The Essential Manual For Every Patient With Atrial Fibrillation
$15.95 (as of April 23, 2025 10:33 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.) The A to Z guide on everything you need to know about atrial fibrillation. Written by AFib expert Dr. Percy Morales MD. Over 120 pages of essential information on medications, procedures, and lifestyles modifications for AFib. Easy to read for every patient.
Shop AFib Products on Amazon
KardiaMobile 6-Lead Personal EKG Monitor – Six Views of The Heart – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Works with Most Smartphones - FSA/HSA Eligible
13% Off
KardiaMobile 1-Lead Personal EKG Monitor – Record EKGs at Home – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Easy to Use – Works with Most Smartphones - FSA/HSA Eligible
$79.00 (as of April 23, 2025 11:23 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display
(as of April 23, 2025 03:02 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Fitbit Sense 2 Advanced Health and Fitness Smartwatch with Tools to Manage Stress and Sleep, ECG App, SpO2, 24/7 Heart Rate and GPS, Shadow Grey/Graphite, One Size (S & L Bands Included)
10% Off
OMRON 2-in-1 Upper Arm Blood Pressure Monitor & 1-Lead EKG Monitor - Clinically Validated Blood Pressure Arm Cuff & Machine - Use OMRON Connect App
32% Off
EMAY Portable ECG Monitor | Record ECG and Heart Rate Anytime Anywhere | Stand-Alone Device with LCD Screen and Storage | No Subscription Required
28% Off
Samsung Galaxy Watch 6 44mm Bluetooth Smartwatch, Fitness Tracker, Personalized HR Zones, Advanced Sleep Coaching, Heart Monitor, BIA Sensor, Health Wellness Insights, Big Screen, US Version, Graphite
27% Off
Natural Rhythm Triple Calm Magnesium 150 mg - 120 Capsules – Magnesium Complex Compound Supplement with Magnesium Glycinate, Malate, and Taurate. Calming Blend for Promoting Rest and Relaxation.
$20.77 ($0.17 / Count) (as of April 23, 2025 11:24 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Pure Encapsulations Magnesium (Glycinate) - Supplement to Support Stress Relief, Sleep, Heart Health, Nerves, Muscles, and Metabolism* - with Magnesium Glycinate - 180 Capsules
$44.60 ($0.25 / Count) (as of April 23, 2025 03:06 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)














![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #1](https://m.media-amazon.com/images/I/311xwtp4mFL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #2](https://m.media-amazon.com/images/I/41j+8AaUGsL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #3](https://m.media-amazon.com/images/I/41jIyxZitnL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #4](https://m.media-amazon.com/images/I/41IpNJERjCL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #5](https://m.media-amazon.com/images/I/31o17yhfYpL._SL100_.jpg)