What is AFib or atrial fibrillation? Understand atrial fibrillation symptoms, causes, and treatment in this comprehensive article.
Did you know that atrial fibrillation (AFib) affects over 33 million people globally, as well as over 5 million across the United States? As a prevalent heart condition, it’s essential to understand what is atrial fibrillation, its symptoms, causes, and available treatment options. Empowering yourself with knowledge about atrial fibrillation can help you take control of your heart health and help you recognize potential warning signs early in your treatment.
In this blog post, we will go through an extensive journey through the world of atrial fibrillation, shedding light on the intricacies of this common heart rhythm disturbance. It’s time to take the driver’s seat in managing your heart health by learning more about atrial fibrillation. By the end of this blog post, you will have a comprehensive understanding of the condition, its diagnosis, treatment options, and preventive measures.
Short Summary
-
Atrial fibrillation is a common heart condition characterized by irregular and rapid heartbeats, which can lead to serious complications if left untreated.
-
Diagnosis of atrial fibrillation requires physical examination, diagnostic tests and in most cases referral to a cardiologist or electrophysiologist.
-
Prevention measures include lifestyle changes such as balanced diet, regular exercise, stress management, weight loss, and mental health care.
Understanding Atrial Fibrillation
Atrial fibrillation, often called AFib, is a common heart condition characterized by irregular and rapid heartbeats. It affects over 33 million people aged 55 and above worldwide, and if left untreated, can lead to the formation of blood clots and increase the risk of stroke and heart failure.
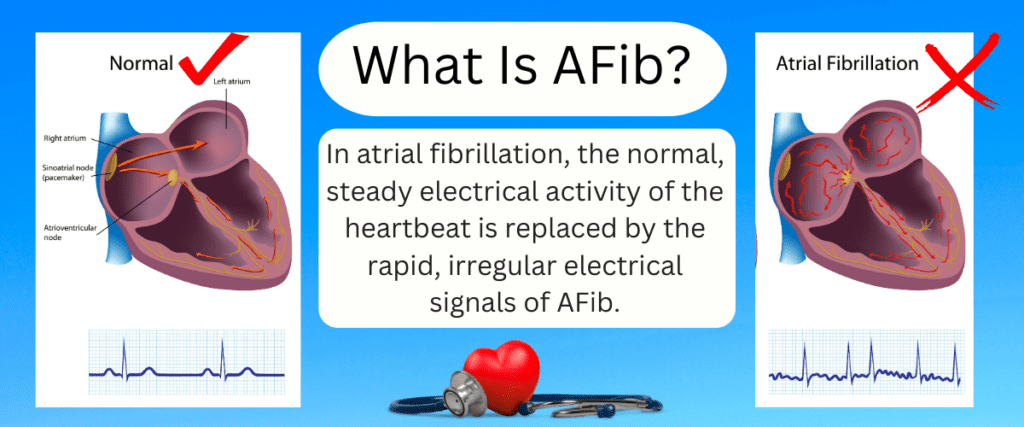
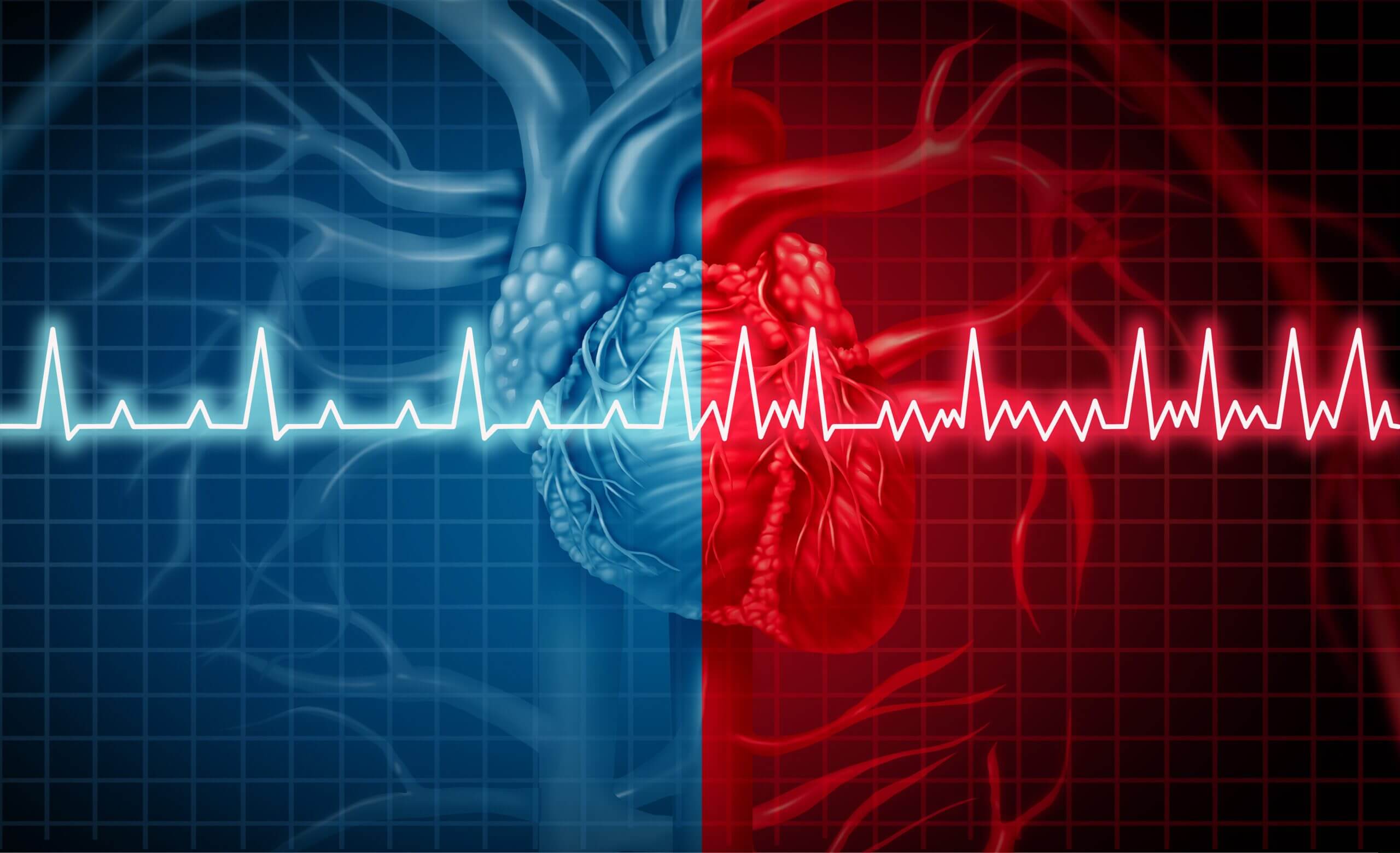
So, what exactly happens during atrial fibrillation? The heart’s upper chambers, known as the atria, contract irregularly and rapidly due to abnormal electrical impulses. This irregular contraction causes the atria to be out of sync with the ventricles, the heart’s lower chambers, resulting in blood pooling in the atrium and increasing the likelihood of blood clot formation. AFib also causes the lower chambers of the heart to beat too quickly and lead to symptoms of a racing heart or heart palpitations. This racing heart can also lead to shortness of breath or heart failure.
Let’s explore how atrial fibrillation occurs and how the different types of AFib that can affect individuals.
How Atrial Fibrillation Occurs
Atrial fibrillation occurs when chaotic electrical impulses in the heart cause the atria to contract irregularly, increasing the risk of blood clots and stroke. These disorganized electrical signals lead to irregular contractions of the atria, disrupting the heart’s natural pacemaker, the sinus node, which is responsible for maintaining a normal rhythm. This results in a rapid and irregular heartbeat, where the atirum quivers very rapidly and the ventricles receive multiple signals trying to reach them.
The impact of atrial fibrillation on an individual’s health can be significant, as irregular heartbeats can lead to blood pooling in the atria, increasing the risk of blood clot formation, and subsequent strokes or other complications. Understanding the different types of AFib and its progression can help guide appropriate treatment approaches and prevent further complications.
Types of Atrial Fibrillation
There are three main types of atrial fibrillation: paroxysmal, persistent, and permanent (also called chronic or long standing persistent), each with varying durations and treatment approaches. Paroxysmal atrial fibrillation typically lasts less than a week and episodes may sometimes resolve on its own without treatment, though it can progress to persistent AFib. Persistent atrial fibrillation continues for more than a week, but less than a year by definition, and frequently requires medical treatment or intervention to reverse back to normal rhythm. Permanent atrial fibrillation lasts for more than a year and also requires long term medical treatment.
Treatment options for atrial fibrillation depend on the type and duration of the condition. Paroxysmal AFib may be treated with medications, lifestyle modifications, or catheter ablation, while persistent AFib may be addressed with medications, cardioversion, catheter ablation, or surgical interventions. Permanent AFib may also be managed with medications, cardioversion, or catheter ablation to reduce the risk of stroke and other complications.
In general, the sooner a patient undergoes treatment for atrial fibrillation, preferably during the paroxysmal atrial fibrillation stage, the more treatment options are available and the better then long term success rate of treatment.
Now that we have a basic understanding of atrial fibrillation and its types, let’s delve into the symptoms and warning signs.
Symptoms and Warning Signs of AFib
The symptoms of atrial fibrillation can vary greatly from person to person, ranging from no symptoms at all to palpitations, fatigue, dizziness, and shortness of breath, depending on the speed of the heart rate. Some individuals may experience heart palpitations, chest pain, dizziness, general fatigue, fluttering or “thumping” in the chest, shortness of breath, weakness, faintness, confusion, and anxiety. It’s crucial to be aware of these symptoms, as recognizing them early can aid in diagnosis and help prevent further complications.
If you or someone you know is experiencing any of these symptoms, it’s essential to seek medical attention promptly. Timely intervention can help manage atrial fibrillation and reduce the risk of stroke and other severe medical issues. But when exactly should you seek medical attention? Let’s find out.
When to Seek Medical Attention
It’s necessary to seek medical attention if you are experiencing severe symptoms of atrial fibrillation. In particular, if you notice severe symptoms such as chest pain, it’s crucial to call emergency services without delay. Delaying medical attention in such cases can worsen the condition and increase the risk of life-threatening complications, such as a heart attack.
In addition to seeking immediate medical attention for severe symptoms, it’s important to consult your healthcare provider for regular check-ups and follow-up appointments post-treatment, as recommended by your doctor. Keeping track of your medications and bringing a list of them to every appointment can help ensure proper management of your atrial fibrillation.
Now, let’s explore the causes and risk factors of atrial fibrillation.
Causes and Risk Factors of AFib
There are some genetic and lifestyle factors that can increase your risk of developing AFib.
Typical AFib risk factors include:
● A history of heart disease (having a past history of a heart attack or congestive heart failure, for example)
● Having uncontrolled high blood pressure
● Living with other chronic health conditions, such as sleep apnea, diabetes, lung disease, or thyroid conditions
● Regularly consuming alcohol
● Having an elevated body mass index (BMI) or Obesity
● Family history of atrial fibrillation
● Advanced age (the incidence of new atrial fibrillation significantly increases after 60 years of age)
While some of these risk factors cannot be changed, all AFib patients need to know that they can improve their symptoms and make disease management easier by making healthier lifestyle choices.
In some cases, the exact cause of atrial fibrillation may remain unknown, but managing these risk factors can help prevent its onset.
Both genetic and environmental factors play a role in the development of atrial fibrillation. Family history can significantly influence the likelihood of developing AFib, as individuals with a close relative diagnosed with the condition are at an increased risk. Let’s take a closer look at the impact of genetics and environmental factors on atrial fibrillation.
Genetic and Environmental Influences
Genetic factors can contribute to the development of atrial fibrillation, with certain individuals being more prone to the condition due to variations inherited from their parents. Studies have identified polymorphisms in several genes, such as KCNQ1, KCNE2, and KCNJ2, as potential risk factors for atrial fibrillation, although a significant portion of the variability in risk remains unexplained.
Environmental factors can also contribute to the development of atrial fibrillation. Prolonged and vigorous endurance exercises, such as swimming and running marathons, can increase the risk of AFib. Additionally, stress, caffeine, and alcohol consumption are associated with an increased risk of atrial fibrillation.
Managing these factors can help in the prevention and management of AFib.
Complications of Atrial Fibrillation
When left untreated, atrial fibrillation can result in some serious complications. Some of the most common complications include:
-
Heart failure — Heart failure occurs when the heart muscle has been damaged. Uncontrolled atrial fibrillation can wear down the heart muscle, resulting in overall poor heart function and heart failure. This can happen when patients have uncontrolled, rapid atrial fibrillation over a period of several weeks or several months.
-
Blood clots — When blood cannot properly circulate from the heart’s atriums, blood clots can form. These clots can result in serious medical emergencies, such as pulmonary embolisms, heart attacks, and strokes.
-
Stroke — People with AFib are at a significantly elevated risk of developing a stroke. A blood clot can form inside the heart during atrial fibrillation which can then travel to the brain and cause a stroke. A stroke is caused by a blood clot becoming lodged in the vessels of the brain, strokes can be an incredibly serious medical condition.
Recent studies have also linked atrial fibrillation to an increased risk of dementia. This association is independent of stroke and other potential risk factors. Let’s further explore the connection between atrial fibrillation and dementia.
The Connection between Atrial Fibrillation and Dementia
Atrial fibrillation has been associated with an elevated risk of dementia, likely due to decreased blood flow to the brain and additional factors. When the heart fails to pump blood effectively due to irregular contractions, the brain may not receive the necessary nutrients and oxygen, leading to cognitive decline over several years and an increased risk of dementia.
While the exact mechanisms behind the connection between atrial fibrillation and dementia remain unclear, understanding this link underscores the importance of timely diagnosis and treatment of AFib to maintain cognitive health and prevent further complications.
Now, let’s discuss how atrial fibrillation is diagnosed and tested.
How is AFib Diagnosed?
Due to the unpredictable nature of atrial fibrillation, it can be difficult to diagnose sometimes, especially in patients that have intermittent episodes that are few and far apart. In general, the main way AFib is diagnosed by your doctor is to have an electrical tracing of your heart during an episode of atrial fibrillation. Here are common methods used to diagnose atrial fibrillation:
-
Electrocardiogram. The electrocardiogram, or ECG or EKG, is the gold standard for determining if someone has atrial fibrillation because it looks at the heart from so many different angles and it’s been used for over 100 years. It commonly offered in a doctors office and gives a detailed snapshot of the electrical activity of the heart.
-
Holter Monitor. A Holter monitor is a continuous heart monitor worn for usually 24-72 hours. These monitors are continuously recording and can help identify intermittent episodes of atrial fibrillation.
-
Event monitor or Mobile Telemetry Monitors. These are extended duration monitors which can be worn from 1 week to up to 4 weeks at a time.
-
Implantable Cardiac Monitor or Loop Recorder. These are very small monitors, about the size of a paperclip, which are implanted underneath the skin. These device are long term monitors that last 3-4 years. They can be very useful diagnose symptoms that are months apart and for the long term management of atrial fibrillation. Learn more about implantable loop recorder monitors here.
-
Home Monitors for AFib Detection. There are several at home monitors that can help you track symptoms of palpitations or atrial fibrillation that do not require a prescription, such as a KardiaMobile device or the Apple Watch. These excellent devices allow you take real time, simplified ECG tracings of your heart rhythm that you can save and show to your doctor. Read my popular KardiaMobile review here.
Treatment Options for Atrial Fibrillation
The treatment options for atrial fibrillation depend on the patient’s health history, symptoms, and preferences. Medical professionals may recommend medications, cardioversion, catheter ablation, or surgical interventions to manage atrial fibrillation and reduce the risk of stroke and other complications. Each treatment approach has its advantages and potential side effects, making it essential to discuss options with a healthcare provider to determine the best course of action for each individual.
Every case of atrial fibrillation is unique. Thetreatmentoptions you may be recommended will depend on multiple factors, such as how long you’ve had the condition, the severity of your symptoms, and any additional health conditions you may have. Some of the most common treatment options include:
Heart Rate Control
Heart rate control usually involves using medications to slow down a rapid heart rate. The most commonly used medications for rate control for AFib include beta-blockers, calcium channel blockers, and digoxin. These medications usually work quickly to slow down a rapid heart rate from AFib and reduce symptoms.
Stroke Risk Reduction
Stroke risk reduction is an essential treatment strategy for anyone living with atrial fibrillation. The primary method for reducing risk of stroke is with blood thinning medications, which can significantly reduce risk of stroke for many patients with AFib. Commonly used blood-thinning medications include:
-
Eliquis
-
Xarelto
-
Pradaxa
-
Savaysa
-
Warfarin
For people who are unable to tolerate standard blood thinning medications, procedural options such as the WATCHMAN procedure have become an excellent option for stroke risk reduction. Learn more about the WATCHMAN procedure here.
Lifestyle Modifications for AFib
All people who live with AFib can reduce their symptoms by living a healthier lifestyle. Participating in regular exercise that you can tolerate, eating a nutritious diet, and getting adequate rest can all play a role in improving your condition. Losing weight, reducing alcohol consumption, treating sleep apnea, and stopping smoking have all been shown to improve symptoms of atrial fibrillation.
Heart Rhythm Control
Many patients with atrial fibrillation will desire a rhythm control strategy (a strategy to return to normal rhythm and reduce risk for AFib recurrence) in order to reduce symptoms of atrial fibrillation. This can be accomplished through a variety of methods.
Medical Therapy
Aggressive heart rhythm medications called anti-arrhythmics can be prescribed under the supervision of an electrophysiologist which may convert a patient out of AFib and keep them in normal rhythm. Some examples of anti-arrhythmic medications include:
-
Flecainide
-
Sotalol
-
Multaq
-
Amiodarone
Cardioversion
Cardioversion is a procedure that uses controlled electric shocks to restore normal heart rhythm, often performed when medications are ineffective in managing atrial fibrillation. During cardioversion, the patient is sedated and an electrical shock is delivered to the chest through electrodes. This shock momentarily stops the heart’s electrical activity, allowing the sinus node to regain control and restore normal heart rhythm. Read more details about a cardioversion procedure here.
While cardioversion can be effective in restoring normal heart rhythm, there is a risk of clot formation associated with the procedure in individuals who have had atrial fibrillation for longer than two days. To reduce this risk, blood-thinning medications such are typically administered for three to four weeks prior to cardioversion and for a minimum of four weeks after the procedure.
Catheter Ablation
A catheter ablation is a minimally invasive procedure where strategic scar is made inside of the heart (usually in the left atrium) where most atrial fibrillation comes from. This strategic scar is created in a way to eliminate or greatly reduce symptoms of AFib. Read more details about catheter ablation procedures here.
Catheter ablation can help restore normal heart rhythm and reduce the symptoms and complications associated with atrial fibrillation. However, it’s essential to discuss the risks and benefits of this procedure with your healthcare provider to determine if it’s the right choice for your unique situation.
Surgical Interventions
In severe cases of atrial fibrillation, more invasive surgical interventions may be necessary to manage the condition and improve symptoms. Surgical procedures, such as the maze procedure, minimally invasive maze surgery (mini-maze), and surgical ablation, involve creating scar tissue to disrupt abnormal electrical signals causing atrial fibrillation.
These surgical interventions can be effective in treating atrial fibrillation, particularly when other treatment options have been unsuccessful. However, as with any surgery, there are more risks and potential complications associated with these procedures. It’s essential to discuss the potential benefits and risks with your healthcare provider before opting for surgical intervention.
Prevention, Lifestyle, and Natural Treatment
Preventing atrial fibrillation involves managing risk factors and making healthy lifestyle choices, such as maintaining a balanced diet, exercising regularly, managing stress, and seeking mental health care. By controlling these factors, individuals can reduce their risk of developing atrial fibrillation and improve their overall heart health.
Adopting healthy habits and making positive lifestyle changes can go a long way in preventing atrial fibrillation and ensuring a healthier life. Let’s explore the specific roles of diet and exercise, as well as stress management and mental health, in preventing atrial fibrillation.
Diet and Exercise
A heart-healthy diet and regular exercise can help reduce the risk of atrial fibrillation by managing weight, blood pressure, and cholesterol levels. Consuming a diet low in saturated fat, trans fat, and cholesterol, and high in fiber, can aid in reducing the risk of atrial fibrillation. Additionally, incorporating the DASH diet, a dietary pattern rich in fruits, vegetables, whole grains, and low-fat dairy products, has been shown to help lower blood pressure and reduce biomarkers of cardiovascular disease.
Regular exercise is also crucial in mitigating the probability of atrial fibrillation by regulating weight, blood pressure, and cholesterol levels. Engaging in physical activity on a regular basis can not only help prevent atrial fibrillation, but also improve overall health and well-being.
Stress Management and Mental Health
Managing stress and maintaining good mental health can also play a role in preventing atrial fibrillation, as anxiety and stress can contribute to cardiovascular disease and cardiac events. Practicing relaxation techniques such as yoga, deep breathing, and meditation can be effective in managing stress and reducing the risk of atrial fibrillation. Small studies have shown that stress management techniques can improve symptoms of atrial fibrillation.
Summary
In conclusion, understanding atrial fibrillation, its symptoms, causes, and available treatments is crucial for maintaining good heart health. By recognizing the warning signs early on, seeking medical attention when necessary, and adopting a heart-healthy lifestyle, individuals can take control of their heart health and prevent the complications associated with atrial fibrillation.
Take charge of your heart health today by making informed decisions about your lifestyle and seeking professional help when needed. Remember, a healthy heart is a happy heart, and the journey to better heart health starts with understanding atrial fibrillation.
Frequently Asked Questions about AFib
What is the main cause of atrial fibrillation?
Atrial fibrillation is most commonly caused by changes to the heart’s tissue or electrical signaling, as well as damage to the heart’s electrical system from other health conditions like hypertension, atherosclerosis, pulmonary embolism, and congenital heart disease.
These conditions can cause the heart to beat irregularly, leading to atrial fibrillation. This can cause symptoms like palpitations, shortness of breath, chest pain, and fatigue. Treatment for atrial fibrillation depends on the underlying cause and the severity of the condition. Medications, lifestyle changes, and medical procedures can all help.
What is the life expectancy of someone with atrial fibrillation?
People with atrial fibrillation may require long-term medications to control the condition. In general, people with atrial fibrillation have a normal life expectancy as long as it is well controlled.
What is atrial fibrillation and is it serious?
Atrial fibrillation (Afib) is a type of arrhythmia where the heart’s upper chambers contract randomly and too fast, causing abnormal electrical impulses to fire in the atria. This can lead to troubling symptoms and serious medical complications, such as blood clots and stroke.
Afib is serious and should be monitored carefully be a cardiologist or electrophysiologist.
What are the warning signs of AFib?
Warning signs of AFib include shortness of breath, heart palpitations, chest pain, fatigue, and lightheadedness.
These symptoms should be taken seriously as they can signify a serious medical issue.
How is atrial fibrillation diagnosed?
Atrial fibrillation is usually diagnosed through physical examination, heart rate and rhythm checks, as well as an electrocardiogram (ECG).
An ECG is a test that records the electrical activity of the heart. It can help detect abnormal heart rhythms, such as atrial fibrillation. It can also help determine the cause of the arrhythmia and the best treatment.
The Best Atrial Fibrillation Book
Your Complete Guide To AFib: The Essential Manual For Every Patient With Atrial Fibrillation
$15.95 (as of April 26, 2024 10:31 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.) The A to Z guide on everything you need to know about atrial fibrillation. Written by AFib expert Dr. Percy Morales MD. Over 120 pages of essential information on medications, procedures, and lifestyles modifications for AFib. Easy to read for every patient.
Shop AFib Products on Amazon
KardiaMobile 6-Lead Personal EKG Monitor – Six Views of The Heart – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Works with Most Smartphones - FSA/HSA Eligible

KardiaMobile 1-Lead Personal EKG Monitor – Record EKGs at Home – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Easy to Use – Works with Most Smartphones - FSA/HSA Eligible

Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display

Fitbit Sense 2 Advanced Health and Fitness Smartwatch with Tools to Manage Stress and Sleep, ECG App, SpO2, 24/7 Heart Rate and GPS, Shadow Grey/Graphite, One Size (S & L Bands Included)

OMRON - Complete Wireless Upper Arm Blood Pressure Monitor + EKG - Built-in Bluetooth Technology

Omron Hem 7361T Bluetooth Digital Blood Pressure Monitor with Afib Indicator and 360° Accuracy Intelliwrap Cuff for Most Accurate Measurements (White)

EMAY Portable ECG Monitor | Record ECG and Heart Rate Anytime Anywhere | Stand-Alone Device with LCD Screen and Storage | No Subscription Required

Samsung Galaxy Watch 6 44mm Smartwatch with HR Zones, Sleep Coaching, Heart Monitor - Graphite

Natural Rhythm Triple Calm Magnesium 150 mg - 120 Capsules – Magnesium Complex Compound Supplement with Magnesium Glycinate, Malate, and Taurate. Calming Blend for Promoting Rest and Relaxation.

Pure Encapsulations Magnesium (Glycinate) - Supplement to Support Stress Relief, Sleep, Heart Health, Nerves, Muscles, and Metabolism* - with Magnesium Glycinate - 180 Capsules

















![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #1](https://m.media-amazon.com/images/I/311xwtp4mFL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #2](https://m.media-amazon.com/images/I/41j+8AaUGsL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #3](https://m.media-amazon.com/images/I/41jIyxZitnL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #4](https://m.media-amazon.com/images/I/41IpNJERjCL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #5](https://m.media-amazon.com/images/I/31o17yhfYpL._SL100_.jpg)