What is paroxysmal AFib and how do you manage its unpredictable episodes? This condition, marked by intermittent and erratic heart rhythms, can be perplexing and concerning. This article aims to demystify paroxysmal AFib (paroxysmal atrial fibrillation) by breaking down its key features, identifying triggers, and outlining practical management strategies – all to help you understand and navigate this condition with clarity.
Key Takeaways
- Paroxysmal Atrial Fibrillation (Also called PAF or Paroxysmal AFib) is a type of heart rhythm disorder that spontaneously starts and stops, there are a variety of treatment options for PAF.
- Common triggers of Paroxysmal AFib include lifestyle factors such as excessive caffeine and alcohol consumption, stress, and insufficient sleep, as well as underlying health conditions like high blood pressure, heart disease, and obesity.
- Management strategies for Paroxysmal AFib encompass medications (e.g., beta-blockers, anticoagulants), lifestyle modifications (e.g., regular exercise, healthy diet), and medical procedures (e.g., catheter ablation, pacemaker implantation) for those who do not respond to medication alone.
Recognizing Paroxysmal AFib Symptoms
Atrial fibrillation is the most common heart arrhythmia, where the heart’s upper chambers – the atria – are fluttering out of sync with the lower ones – the ventricles. When atrial fibrillation occurs, leading to an irregular and rapid heartbeat, it is often described as ‘fluttering’ or ‘quivering’. But not all AFib is the same. Sometimes atrial fibrillation can be paroxysmal AFib, which comes and goes, usually resolving within a week, either spontaneously or with treatment. In some cases, patients can have persistent atrial fibrillation, where episodes last longer then 7 days. Alternatively, some patients may alternatively experience atrial flutter, a related but distinct condition in the heart’s upper chambers.
But how does paroxysmal AFib differ from other types of AFib? To understand this, we’ll dig deeper into the nature of paroxysmal AFib and compare it to its counterparts. Shall we?
Definition and characteristics
Paroxysmal AFib is a subtype of atrial fibrillation, a heart rhythm disorder characterized by an irregularly irregular heart rhythm. It’s like a dance that starts and stops without notice. Some episodes resolve on their own, while others persist, requiring medical intervention to restore the heart’s rhythm.
Imagine a mischievous spark causing chaos in the heart’s rhythm. This spark often lurks in the left atrial muscular sleeve extending into the pulmonary vein, the most common site for extra beats that can trigger paroxysmal AFib.
Comparison to other types of AFib
In contrast to the intermittent episodes of paroxysmal AFib, persistent atrial fibrillation is like a dance that never stops. The irregular heartbeat is constant, yet individuals can still engage in activities like exercise, provided their heart rate is well-controlled and they are stable on treatment.
It’s like comparing a pop-up storm to a persistent drizzle. Both are forms of rainfall, but they occur differently. Similarly, both paroxysmal AFib and persistent AFib are forms of the same irregular heart rhythm, but they present differently. Understanding these differences is crucial in managing the condition and mitigating its impacts.
Identifying Symptoms of Paroxysmal Atrial Fibrillation
Imagine feeling your heart flutter or racing like a trapped bird in your chest. Or experiencing sudden onset of shortness of breath, dizziness, and chest pain without any apparent reason. These could be signals from your body, symptoms of paroxysmal atrial fibrillation. But what if you don’t feel any of these symptoms? Can you still have paroxysmal AFib?
To answer these questions, we’ll explore the typical symptoms of paroxysmal AFib and delve into the phenomenon of asymptomatic cases. Because sometimes, what you don’t feel can still affect you.
Typical symptoms
Imagine feeling:
- dizzy or lightheaded out of the blue
- experiencing a sudden chest pain that leaves you feeling unwell
- feeling your heart racing, pounding hard against your chest wall, like a drumbeat gone rogue
- some patients may have no recognizable symptoms
Recognizing AFib symptoms, also known as symptoms of atrial fibrillation, is crucial, especially when dealing with paroxysmal AFib.
In addition, you might experience a wave of fatigue washing over you or shortness of breath that leaves you gasping for air. These symptoms may come and go, making it challenging to associate them with a heart condition. But awareness of these signs is the first step towards early detection and management of paroxysmal AFib.
Asymptomatic cases
It’s possible to have paroxysmal AFib and not know it. Like a thief in the night, this condition can sneak up on you without any noticeable symptoms. In fact, a significant percentage of patients, have been found to experience at least one period of asymptomatic paroxysmal AFib.
Despite being on medical therapy, many patients may continue to have asymptomatic episodes of paroxysmal atrial fibrillation, potentially progressing to persistent atrial fibrillation. This makes regular medical examinations crucial for detecting and monitoring paroxysmal AFib and preventing its potential complications. You may not feel the storm, but that doesn’t mean it’s not there.
Common Triggers and Risk Factors
Just as a spark can ignite a fire, certain triggers can set off paroxysmal AFib. These triggers, which include lifestyle choices and health conditions, can increase the risk of developing the condition. But how exactly do these factors trigger paroxysmal AFib? And how can you mitigate these risks?
To answer these questions, we’ll explore the lifestyle-related triggers and health conditions associated with paroxysmal AFib. Because when it comes to managing this condition, prevention is often the best cure.
Lifestyle-related triggers of Paroxysmal AFib
Ever noticed how drinking too much coffee can make your heart race? Or how a stressful day can leave you feeling like your heart is about to burst out of your chest? These are examples of how lifestyle choices can trigger paroxysmal AFib.
A lack of sufficient sleep, and high-stress levels can potentially trigger episodes of paroxysmal atrial fibrillation. But all is not lost. Implementing the following practices can help control blood pressure and reduce the frequency of AFib episodes:
- Engage in stress-reducing activities such as meditation, yoga, or deep breathing exercises.
- Limit the intake of caffeine and alcohol, as they can contribute to AFib episodes.
- Get enough sleep and establish a regular sleep schedule.
- Maintain a healthy diet and exercise routine.
- Take prescribed medications as directed by your doctor.
It’s about finding a balance that works for your body.
Health conditions and risk for Paroxysmal AFib
Underlying health conditions that can increase the risk of developing paroxysmal AFib include:
- High blood pressure
- Heart disease
- Thyroid problems
- Sleep apnea
- Chronic lung disease
- Diabetes
- Obesity
- Chronic kidney disease
- Alcohol abuse
- Stimulant use (such as caffeine or certain medications)
Also, several underlying health conditions can wreak havoc on the heart’s structure and negatively impact the electrical pulses that govern the heartbeat, leading to paroxysmal atrial fibrillation.
Risk factors for atrial fibrillation include:
- Obesity
- Diabetes
- Heart failure
- Ischemic heart disease
- Valvular heart disease
- Hyperthyroidism
- Chronic kidney disease
- Enlargement of the left heart chambers
- Age (prevalence increases in older populations)
- Additional health conditions like diabetes, thyroid problems, and pericarditis
- Long-term exposure to air pollution
- Obstructive sleep apnea
These factors are associated with a higher likelihood of developing paroxysmal atrial fibrillation.
But knowledge is power, and being aware of these risk factors can empower you to take proactive steps towards disease prevention.
Diagnosis and Monitoring of Paroxysmal AFib
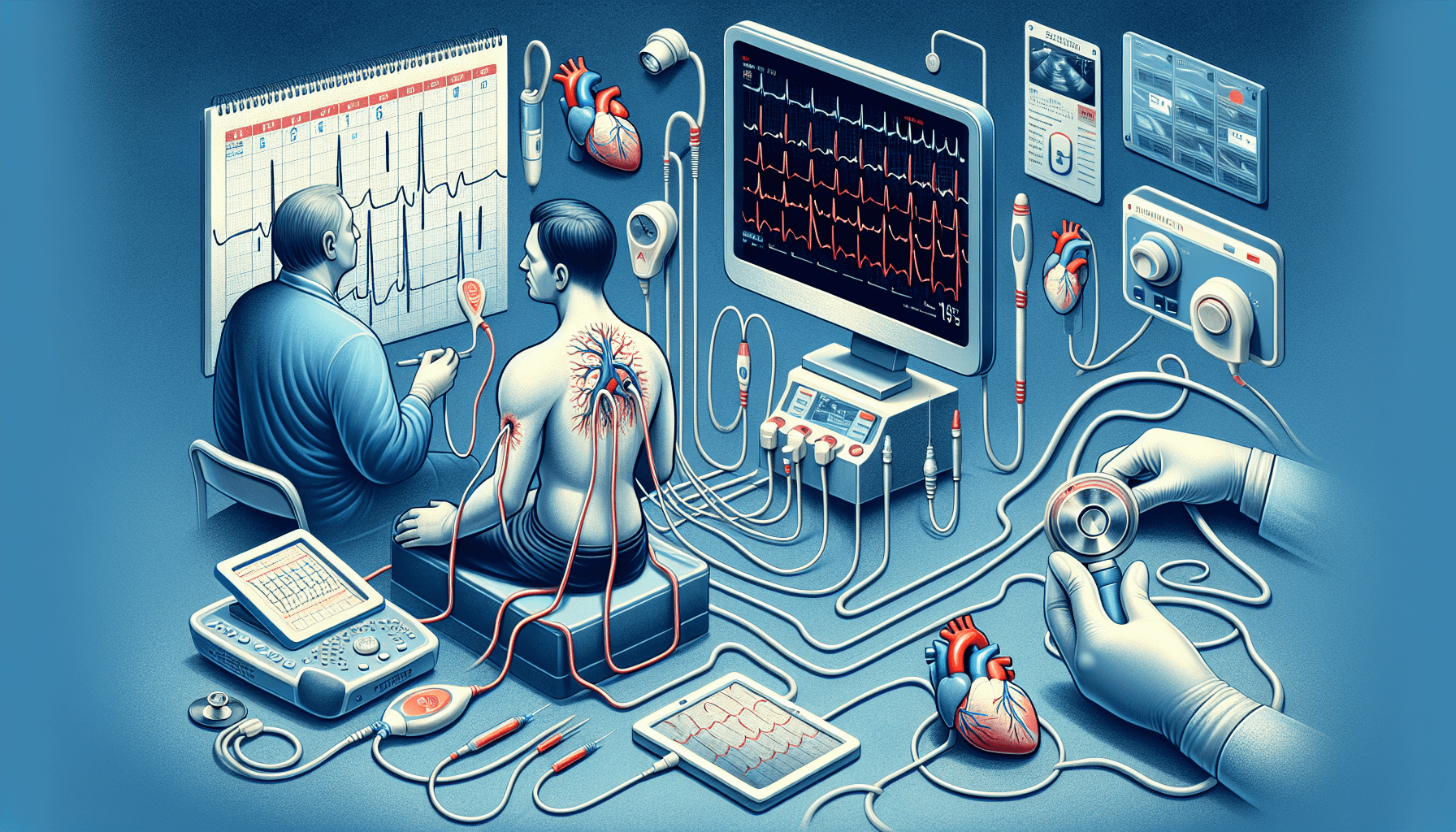
If paroxysmal AFib is a storm, then diagnostic tests and monitoring are the radar that detects it. Extended ECG monitoring periods, like 14 days, are crucial to catch less frequent, but clinically important, paroxysmal atrial fibrillation episodes. But how do these diagnostic tests work? And how can you monitor your condition?
Let’s explore the tools available for diagnosis and monitoring of paroxysmal AFib, from extended ECG monitoring to digital technology advancements, and the importance of regular check-ups and self-monitoring.
Diagnostic tests
Imagine wearing a patch that can monitor your heart rhythm for 14 days straight. Advances in ambulatory Holter monitors have made this possible, with patient-friendly features like waterproofing and wireless communication enhancing their utility for cardiac rhythm monitoring.
14-day ECG patch monitors have been shown to have a higher detection rate for paroxysmal arrhythmias compared to a standard 24-hour Holter monitor. Additionally, handheld ECG recorders compatible with smartphones, such as KardiaMobile and Apple Watch, have made it possible to diagnose atrial fibrillation easily and swiftly.
Long-term continuous ECG monitoring with a 14-day patch supports atrial fibrillation diagnosis, as it helps identify asymptomatic episodes of silent atrial fibrillation, which are not uncommon and can carry important clinical consequences.
Regular check-ups and self-monitoring
Regular doctor visits are crucial for individuals with paroxysmal AFib to manage their condition. Just as you would service a car regularly to keep it running smoothly, regular check-ups can help in the early detection of arrhythmia episodes and any potential complications.
But what about those times in between doctor visits? That’s where self-monitoring comes in. Patients with paroxysmal AFib should be educated on how to self-monitor their pulse to check for irregular heartbeats and contact a healthcare provider as needed. Incorporating pulse self-monitoring into daily routine allows for timely detection and treatment of AFib episodes. Also, handheld ECG recorders compatible with smartphones, such as KardiaMobile and Apple Watch, have been useful in the tracking of AFib episodes.
Treatment and Management Strategies
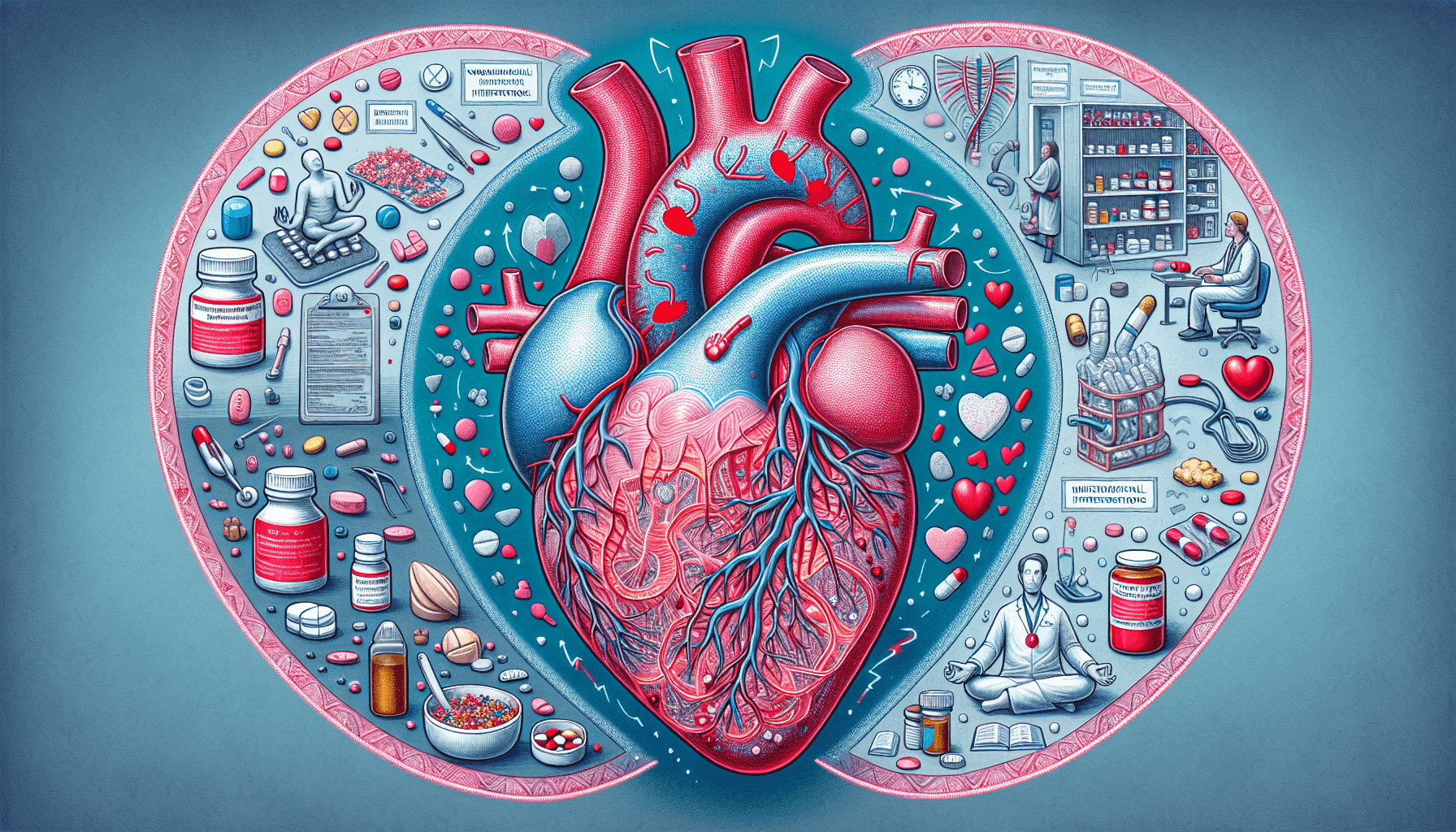
Even as a storm rages, there are ways to bring calm. Maintaining a well-controlled atrial fibrillation treatment plan is crucial for individuals with AFib to prevent complications and live an active life. But what does this treatment plan entail?
From medications to non-pharmacological interventions and medical procedures, let’s explore the arsenal of strategies available for managing paroxysmal AFib.
Medications
Medications play a crucial role in managing paroxysmal AFib. They are like the anchors that keep the dancing heart in rhythm. Beta-blockers and calcium channel blockers are used to slow the heart rate in patients with paroxysmal atrial fibrillation, and can help prevent episodes of Paroxysmal AFib.
Some individuals may require anti-arrhythmic medications such as sodium channel blockers and potassium channel blockers to maintain a normal heart rhythm. And to reduce the risk of blood clots and stroke, anticoagulants, also known as blood thinners, are often prescribed to individuals with paroxysmal atrial fibrillation.
It’s all about keeping the rhythm while preventing any potential complications including risk of stroke.
Non-pharmacological interventions
Aside from medications, lifestyle modifications can go a long way in managing paroxysmal AFib. They are the everyday choices that can make a big difference. Here are some recommended lifestyle modifications for patients with paroxysmal atrial fibrillation:
- Managing cholesterol
- Controlling blood pressure
- Maintaining a healthy weight
- Avoiding excessive alcohol and caffeine consumption
- Engaging in regular exercise
These lifestyle modifications can help in managing paroxysmal AFib effectively.
For those who smoke, quitting is advised, and resources like tobacco cessation programs are available to assist them. After all, it’s not just about treating the condition; it’s about embracing a healthier lifestyle that supports overall well-being.
Medical procedures
When medications and lifestyle changes aren’t enough, medical procedures step in to pick up the slack. Procedures like catheter ablation, including radiofrequency ablation or cryoablation, are utilized to restore normal heart rhythm in patients with paroxysmal atrial fibrillation who do not respond adequately to medication.
Read my comprehensive guide on AFib Ablation here.
For patients where medications or less invasive procedures fail, surgical options such as the Maze procedure, mini maze, and the convergent procedure may be considered.
Living with Paroxysmal Atrial Fibrillation
Living with paroxysmal AFib is like sailing in a stormy sea. It can be challenging, but with the right tools and guidance, it’s possible to navigate the storm safely. From managing exercise and travel considerations to self-monitoring, individuals with paroxysmal AFib can lead active and fulfilling lives.
Let’s explore how you can manage exercise, travel, and self-monitoring while living with paroxysmal AFib. Because being diagnosed with paroxysmal AFib is not the end of the journey, but the beginning of a new chapter.
Exercise and physical activity
While living with paroxysmal AFib, exercise can be a double-edged sword. On one hand, regular physical activity helps control modifiable risk factors like hypertension and overweight, and independently reduces the likelihood of AFib occurrences. On the other hand, excessive physical activity, especially in endurance sports, might trigger AFib in individuals due to associated structural and electrophysiological heart alterations.
The key is to find a balance. Moderate-intensity physical activity is recommended to decrease AFib occurrences, with a focus on exercises like:
- brisk walking
- swimming
- cycling
- resistance training
And during periods without irregular heartbeats, individuals with paroxysmal AFib can participate in safe exercise routines, after taking appropriate precautions.
Travel considerations
Traveling with paroxysmal AFib can be like carrying an extra suitcase. It requires a bit more preparation, but with the right planning, it’s entirely manageable. Before traveling, individuals with paroxysmal atrial fibrillation should seek their doctor’s advice on managing their condition and be prepared for potential medical emergencies.
When traveling with paroxysmal atrial fibrillation, it is important to:
- Carry a sufficient supply of medications
- Keep your healthcare provider’s contact information accessible
- Engage in walking and standing exercises during long flights to prevent blood clots
- Wear compression stockings to further reduce the risk of blood clots
With these considerations in mind, individuals with paroxysmal AFib can enjoy their travel experiences without unnecessary worry.
Summary
From the onset of the journey, we’ve delved into the world of paroxysmal atrial fibrillation. We’ve explored its characteristics, identified its symptoms, and highlighted its triggers and risk factors. We’ve discovered the tools for its diagnosis and monitoring, and discussed the various methods for its treatment and management. We’ve also learned how to live with paroxysmal AFib, from managing exercise and travel to self-monitoring.
But the journey doesn’t end here. Knowledge is power, and being equipped with this understanding of paroxysmal atrial fibrillation empowers you to take proactive steps towards managing this condition. It’s all about finding your rhythm in the storm and turning the tide of paroxysmal AFib.
Frequently Asked Questions
What is paroxysmal atrial fibrillation?
Paroxysmal atrial fibrillation is a subtype of atrial fibrillation characterized by episodes of irregular heart rhythm that start and stop spontaneously, often resolving within 7 days. It is a temporary condition that may require treatment to manage symptoms.
What are the typical symptoms of paroxysmal atrial fibrillation?
Typical symptoms of paroxysmal atrial fibrillation include palpitations, shortness of breath, fatigue, chest pain, and dizziness. Some individuals may not experience any symptoms.
What are the common triggers and risk factors for paroxysmal atrial fibrillation?
Common triggers and risk factors for paroxysmal atrial fibrillation include lifestyle choices such as excessive caffeine and alcohol consumption, stress, and lack of sleep, as well as health conditions like high blood pressure, heart disease, obesity, diabetes, and age. These can increase the likelihood of experiencing AFib.
How is paroxysmal atrial fibrillation diagnosed and monitored?
Diagnosis and monitoring of paroxysmal atrial fibrillation involve extended ECG monitoring, diagnostic tests like ambulatory Holter monitors and ECG patch monitors, and regular check-ups and self-monitoring. It’s important to use these methods consistently to effectively manage the condition.
What are some treatment and management strategies for paroxysmal atrial fibrillation?
The treatment and management strategies for paroxysmal atrial fibrillation include medications, non-pharmacological interventions, and medical procedures such as ablation or surgery. It’s important to work with a healthcare professional to determine the most effective approach for your specific condition.
The Best Atrial Fibrillation Book
Your Complete Guide To AFib: The Essential Manual For Every Patient With Atrial Fibrillation

Shop AFib Products on Amazon
KardiaMobile 6-Lead Personal EKG Monitor – Six Views of The Heart – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Works with Most Smartphones - FSA/HSA Eligible
13% Off
KardiaMobile 1-Lead Personal EKG Monitor – Record EKGs at Home – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Easy to Use – Works with Most Smartphones - FSA/HSA Eligible
$79.00 (as of June 14, 2025 15:10 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display
(as of June 14, 2025 08:29 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Fitbit Sense 2 Advanced Health and Fitness Smartwatch with Tools to Manage Stress and Sleep, ECG App, SpO2, 24/7 Heart Rate and GPS, Shadow Grey/Graphite, One Size (S & L Bands Included)
20% Off
OMRON 2-in-1 Upper Arm Blood Pressure Monitor & 1-Lead EKG Monitor - Clinically Validated Blood Pressure Arm Cuff & Machine - Use OMRON Connect App
21% Off
Samsung Galaxy Watch 6 44mm Bluetooth Smartwatch, Fitness Tracker, Personalized HR Zones, Advanced Sleep Coaching, Heart Monitor, BIA Sensor, Health Wellness Insights, Big Screen, US Version, Graphite
9% Off
Natural Rhythm Triple Calm Magnesium 150 mg - 120 Capsules – Magnesium Complex Compound Supplement with Magnesium Glycinate, Malate, and Taurate. Calming Blend for Promoting Rest and Relaxation.
$20.77 ($0.17 / Count) (as of June 14, 2025 17:38 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Pure Encapsulations Magnesium (Glycinate) - Supplement to Support Stress Relief, Sleep, Heart Health, Nerves, Muscles, and Metabolism* - with Magnesium Glycinate - 180 Capsules
$44.60 ($0.25 / Count) (as of June 14, 2025 08:29 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)














![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #1](https://m.media-amazon.com/images/I/311xwtp4mFL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #2](https://m.media-amazon.com/images/I/41j+8AaUGsL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #3](https://m.media-amazon.com/images/I/41jIyxZitnL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #4](https://m.media-amazon.com/images/I/41IpNJERjCL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #5](https://m.media-amazon.com/images/I/31o17yhfYpL._SL100_.jpg)