Are you or a loved one living with atrial fibrillation and worried about stroke risk? The Watchman implant offers strategic stroke prevention. Specifically designed for AFib patients at risk for stroke, this implant provides an alternative to long-term blood thinners by sealing off the left atrial appendage, a common site for clot formation and stroke risk. Learn if you’re a candidate, understand the implantation process, and explore the benefits and risks in this detailed guide.
Key Takeaways
-
The WATCHMAN device is a minimally invasive implant designed to prevent strokes in patients with non-valvular atrial fibrillation by occluding the left atrial appendage, thereby reducing the need for lifelong anticoagulation therapy.
-
The WATCHMAN implantation procedure is usually performed under general anesthesia or sedation, involves precise imaging guidance, and requires post-procedure care including a regimen of anticoagulants or antiplatelets and short term limitations on physical activity for optimal recovery.
-
While the WATCHMAN device offers significant long-term benefits, including stroke reduction and improved quality of life without the need for strong blood thinning medication, potential risks such as peri-device leaks, tissue perforation, and device dislodgement must be carefully considered and require qualified medical implanters for the procedure.
Understanding the WATCHMAN Device
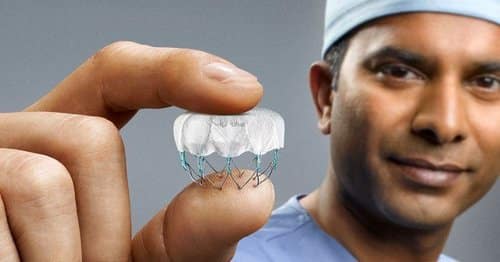
For those living with the fear of stroke due to atrial fibrillation, the WATCHMAN device provides hope for a life without strong blood thinning medications. This small, self-expanding device is the answer to a monumental problem, reducing stroke risk by occluding the left atrial appendage—the main site for blood clot formation in AFib patients.
The closure of the left atrial appendage (LAA) with the WATCHMAN device offers several benefits for AFib patients:
-
It eliminates the necessity for life-long anticoagulation therapy.
-
It offers patients a renewed sense of freedom and a chance at a healthier, worry-free future.
-
One time procedure that does not need to be replaced.
The Mechanics Behind the WATCHMAN
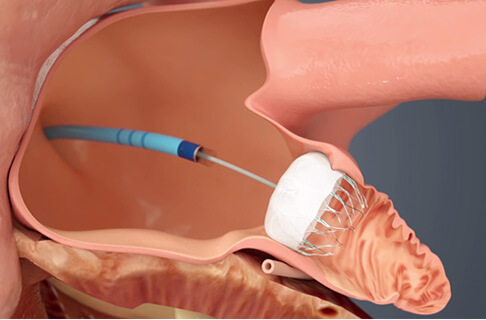
By creating a seal in the left atrial appendage, the WATCHMAN device inhibits blood clot formation and their migration into the bloodstream. The left atrial appendage serves as the primary site for blood clot formation in AFib patients. By sealing this appendage, the atrial appendage device implantation effectively stops the migration of these clots into the bloodstream, reducing the risk of stroke.
Think of the WATCHMAN device as a tiny plug standing guard at the entrance of the left atrial appendage. Its mission? To block blood clots from escaping the appendage and causing stroke in AFib patients. This simple, minimally invasive, yet effective mechanism has proven to be a promising solution for stroke prevention in AFib patients.
Who Should Consider the WATCHMAN Implant?
The WATCHMAN procedure is not a one-size-fits-all solution—it’s specifically designed for a certain group of individuals. Patients with non-valvular atrial fibrillation exploring alternatives to blood thinners are prime candidates for the procedure.
But how does one know if they’re an ideal candidate? Several factors are considered when selecting patients for the WATCHMAN procedure. These include:
-
A history of major or non-major bleeding on anticoagulation
-
A high risk of future bleeding
-
Contraindication to oral anticoagulation, such as a blood thinner
-
Intolerance to oral anticoagulation
-
An increased risk for stroke based on CHADS2 score or CHA2DS2-VASc score.
The WATCHMAN Procedure: A Step-by-Step Guide
The WATCHMAN procedure involves a series of meticulously coordinated steps. It begins with pre-procedure assessments, leading to a minimally invasive implantation process, and culminates in post-procedure care. The procedure involves creating a small incision in the groin, introducing a catheter through a blood vessel up to the heart, using imaging to direct the catheter to the correct position, identifying the preferred WATCHMAN size, and implanting the WATCHMAN device into the left atrial appendage.
Imaging plays a crucial role in the procedure, assisting in guiding the catheter to the appropriate position, and sizing the correct device. The type of anesthesia administered during the procedure varies between sedation and full anesthesia, based on the center’s preference. This is primarily to optimize patient comfort during the performance of transesophageal echocardiography (TEE), which is frequently utilized for procedural guidance.
Pre-Procedure Assessments
Patients usually undergo a comprehensive screening before the procedure. This may include transesophageal echocardiography (TEE) or a contrast 64-slice cardiac CT scan. These assessments aid in the planning of the implantation and anatomical analysis of the left atrial appendage (LAA).
The pre-procedural TEE is critical to rule out the presence of a left atrial appendage (LAA) thrombus and evaluate the suitability of LAA ostium dimensions for closure with the Watchman device, which is one of a few atrial appendage occlusion procedures. Sometimes a TEE is performed the same morning as the planned WATCHMAN implant.
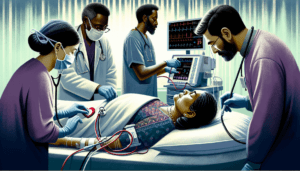
During the Procedure
Usually performed under general anesthesia, the WATCHMAN procedure includes the following steps:
-
Access is gained through usually the right femoral vein.
-
Catheters are first advanced to the right atrium
-
A transeptal puncture if performed, crossing from the right atrium to left atrium using ultrasound guidance, from either a TEE or intracardiac echo.
-
The WATCHMAN sheath is advanced into the left atrial appendage.
-
After determining the ideal size, the WATCHMAN implant is advanced and then deployed into the left atrial appendage.
-
The implant undergoes a series of tests on ultrasound or TEE, and xray to determine satisfactory size and position in the LAA are met.
-
If satisfactory, then the WATCHMAN implant is released from the connected catheter and left in place, the procedure is then completed.
The WATCHMAN implant procedure usually takes less then 1 hour to perform. Most patients are able to go home the same day as the procedure after a few hours of bedrest in a procedure recovery area.
Post-WATCHMAN Implant Care and Recovery
The journey continues even after the WATCHMAN device has been implanted, with post-procedure care being crucial for optimal functioning of the device and swift patient recovery.
This involves medication management, adhering to a recovery timeline, and following prescribed activity recommendations.
Medications After WATCHMAN
Post-procedure medication management is a critical aspect of recovery. Typical anticoagulants recommended following the WATCHMAN procedure are clopidogrel and aspirin, or a combination of anticoagulation and aspirin, based on doctor’s preferences. Patients are advised to undergo dual anti-platelet therapy for approximately 6 months following the procedure.
Dual anti-platelet therapy (DAPT) is a commonly employed antithrombotic regimen subsequent to the WATCHMAN procedure. It is instrumental in mitigating the risk of bleeding, particularly following the cessation of warfarin and the temporary utilization of DAPT.
Furthermore, a low-dose daily aspirin is recommended long term, approximately 6 months after the to mitigate the risk of blood clots and stroke.
Recovery Timeline and Activity Recommendations
After the procedure, patients typically experience a recovery period of 2-4 hours and are usually able to return home on the same day. However, it is important for them to adhere to strict limitations on strenuous activity for the initial week.
Patients are advised to gradually resume normal activities of daily living approximately 24 hours after the procedure. However, strenuous activities, such as heavy lifting, should be avoided for a few weeks to facilitate proper recovery post the WATCHMAN procedure.
Advantages and Longevity of the WATCHMAN Device
The benefits of the WATCHMAN device include:
-
Immediate effect in improving the quality of life for AFib patients
-
Lifelong functionality without the need for replacement. One time procedure.
-
Long-term protection against stroke without strong blood thinning medications.
These benefits make the WATCHMAN device a valuable and convenient option for AFib patients.
The WATCHMAN device is regarded as a long-term solution for stroke prevention due to its ability to offer a one-time protection by closing off the left atrial appendage, the primary location for the formation of stroke-causing clots. Research has shown its sustained safety and effectiveness in not only reducing strokes but also minimizing bleeding and mortality in comparison to long-term warfarin therapy.
Life with the WATCHMAN: Long-Term Benefits
The WATCHMAN device doesn’t just offer a solution—it offers a lifestyle change. Clinical studies have demonstrated the efficacy of the WATCHMAN device in reducing the risk of stroke and mortality.
Moreover, the WATCHMAN device mitigates the risk of bleeding and is equally efficacious as medication in lowering the risk of stroke, consequently reducing the long-term dependency on medication. Research indicates that the WATCHMAN device has demonstrated a substantial enhancement in the quality of life for AFib patients. The studies have revealed positive developments in physical functioning and overall quality of life following the 12-month period post-implantation.
Risks and Considerations
As with all medical procedures, the WATCHMAN procedure carries its own set of risks and considerations. Potential complications may include peri-device leaks, which could occur as a result of size and shape discrepancies between the device and the left atrial appendage (LAA) ostium. There is some data demonstrating that even small peri-device leaks can increase risk of stroke post WATCHMAN implant.
Choosing the right implanting physician is an important consideration. The WATCHMAN procedure should be performed by a healthcare provider with specific qualifications such as an interventional cardiologist, electrophysiologist, or cardiovascular surgeon. It is advisable to inquire about the number of procedures they have performed, their success rate, any encountered complications, their tenure in performing the procedure, and specific patient criteria or qualifications for the procedure.
Recognizing Potential Complications
Complications may arise during the WATCHMAN procedure, including:
-
Heart tissue perforation
-
Reactions to anesthesia
-
Infection at the catheter insertion site
-
Potential device dislodgment
It’s crucial for patients to be aware of these potential complications, and be aware of signs of complications.
For instance, infection at the catheter insertion site can be identified through symptoms such as redness, swelling, or the presence of pus. Additionally, in some instances, a hematoma may develop around the insertion site. Reactions to anesthesia during the WATCHMAN procedure can vary, with both conscious sedation and general anesthesia having similar device success rates and safety outcomes.
It’s crucial to monitor for peri-device leaks 45 to 90 days following the procedure. Usually some type of post procedure imaging is performed to assess for peri-device leaks such as a TEE or Cardiac CTA. If complications are detected, they are usually managed by implanting physician. Some patients may continue to take stronger anticoagulation medications for a period of time after a WATCHMAN implant due to a peri-device leak. However, previous studies have demonstrated that most peri-device leaks are sealed within 1 year after procedure.
Choosing the Right Medical Provider
Choosing the right medical provider to perform the WATCHMAN procedure is as vital as the procedure itself. The qualifications required for a healthcare provider to perform the procedure include being an interventional cardiologist, electrophysiologist, or cardiovascular surgeon.
When assessing a potential provider’s experience with the WATCHMAN procedure, it’s advisable to inquire about:
-
The number of procedures they have performed
-
Their success rate
-
Any encountered complications
-
Their tenure in performing the procedure
-
Specific patient criteria or qualifications for the procedure
The typical success rate for healthcare providers performing the WATCHMAN procedure varies from 94% to 100%.
Real-World Effectiveness: Clinical Trials and Patient Outcomes
Transitioning from theory to practice, we will explore the practical effectiveness of the WATCHMAN device. Clinical trials on this device have demonstrated the effectiveness of left atrial appendage closure (LAAC) with Watchman in preventing strokes in patients with non-valvular AF. Furthermore, patients who have undergone the WATCHMAN procedure have reported success rates ranging from 94% to 100%.
The OPTION trial signifies essential ongoing research aimed at addressing anticoagulation management and stroke prevention strategy post-ablation for patients with nonvalvular atrial fibrillation. Its findings could potentially impact future treatment guidelines and patient care protocols.
Success Stories and Testimonials
The transformative impact of the procedure is evident in the success stories of patients who have received the WATCHMAN device implant, which can be found on various platforms. Testimonials of patients are available on the official WATCHMAN website featuring patient that share the success of their WATCHMAN implant.
Long-term testimonials from patients who have been living with the WATCHMAN device shed light on the lasting impact of the procedure. These patients have shared their experiences of living without the need for long-term oral anticoagulation (OAC) and reducing their AFib-related stroke risk.
Summary
In summary, the WATCHMAN device is a significant innovation that is transforming lives by offering an effective, long-term solution for stroke prevention in AFib patients. Its mechanics, the intricacies of the procedure, and the comprehensive post-implant care ensure a high success rate and improved quality of life. While potential risks and complications exist, selecting the right medical provider can mitigate these risks. Real-world effectiveness, as demonstrated by clinical trials and patient outcomes, underscores the device’s potential in revolutionizing stroke prevention.
Frequently Asked Questions
What does the watchman implant do?
The WATCHMAN implant prevents blood clots from forming in the left atrial appendage (LAA) by acting as a small parachute-shaped device, about the size of a quarter, that blocks off this area.
What are the negatives for a Watchman device?
Some possible complications of the Watchman procedure include clot formation and device-related thrombus. It’s important to discuss these risks with your healthcare provider.
How long does a watchman implant last?
The WATCHMAN Implant lasts for a lifetime once it’s placed in your heart. It’s a permanent implant that doesn’t need to be replaced.
Does watchman get rid of AFib?
The Watchman device is an implant for reducing stroke risk in patients with non-valvular atrial fibrillation. It specifically targets the left atrial appendage and does not impact the frequency or duration of atrial fibrillation. Read more about AFib treatments here.
What is the WATCHMAN device?
The WATCHMAN device is an FDA-approved atrial appendage closure device that helps reduce stroke risk in patients with AFib.
The Best Atrial Fibrillation Book
Your Complete Guide To AFib: The Essential Manual For Every Patient With Atrial Fibrillation

Shop AFib Products on Amazon
KardiaMobile 6-Lead Personal EKG Monitor – Six Views of The Heart – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Works with Most Smartphones - FSA/HSA Eligible
13% Off
KardiaMobile 1-Lead Personal EKG Monitor – Record EKGs at Home – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Easy to Use – Works with Most Smartphones - FSA/HSA Eligible
$79.00 (as of June 17, 2025 07:57 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display
(as of June 17, 2025 08:55 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Fitbit Sense 2 Advanced Health and Fitness Smartwatch with Tools to Manage Stress and Sleep, ECG App, SpO2, 24/7 Heart Rate and GPS, Shadow Grey/Graphite, One Size (S & L Bands Included)
10% Off
OMRON 2-in-1 Upper Arm Blood Pressure Monitor & 1-Lead EKG Monitor - Clinically Validated Blood Pressure Arm Cuff & Machine - Use OMRON Connect App
24% Off
Samsung Galaxy Watch 6 44mm Bluetooth Smartwatch, Fitness Tracker, Personalized HR Zones, Advanced Sleep Coaching, Heart Monitor, BIA Sensor, Health Wellness Insights, Big Screen, US Version, Graphite
$353.21 (as of June 17, 2025 07:57 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Natural Rhythm Triple Calm Magnesium 150 mg - 120 Capsules – Magnesium Complex Compound Supplement with Magnesium Glycinate, Malate, and Taurate. Calming Blend for Promoting Rest and Relaxation.
$20.77 ($0.17 / Count) (as of June 17, 2025 07:57 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Pure Encapsulations Magnesium (Glycinate) - Supplement to Support Stress Relief, Sleep, Heart Health, Nerves, Muscles, and Metabolism* - with Magnesium Glycinate - 180 Capsules
$44.60 ($0.25 / Count) (as of June 17, 2025 08:55 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)














![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #1](https://m.media-amazon.com/images/I/311xwtp4mFL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #2](https://m.media-amazon.com/images/I/41j+8AaUGsL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #3](https://m.media-amazon.com/images/I/41jIyxZitnL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #4](https://m.media-amazon.com/images/I/41IpNJERjCL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #5](https://m.media-amazon.com/images/I/31o17yhfYpL._SL100_.jpg)