Read more about what to do if you have AFib after ablation in this article. There are many people that continue to struggle with episodes of atrial fibrillation, even despite past procedures such as an ablation. Many people have gone through this, and perhaps you have gone through this too, where you have already gone through an experience of an ablation procedure, you went through sometimes a challenging recovery period as well, and then afterwards find that you are still having episodes of atrial fibrillation. Hopefully the symptoms are better than it was prior to the ablation, but it’s possible that your control is not as satisfactory as you would like it to be.
Can Atrial Fibrillation Come Back After Ablation?
In this article I will discuss some of the reasons why people still have AFib after an ablation procedure, and what you can do to help improve your success rate of an ablation procedure. When it comes to the reasons why an ablation procedure does not work, I’ll divide it up into technical failures as well as what I would call “missing pieces of the puzzle.”
When it comes to technical failures, that basically means that there was an incompleteness or an issue with the actual ablation procedure itself. It can be because areas grow back from the original procedure, which I’m going to discuss more below, or it could be that not enough was ablated at that time.
Your Complete Guide To AFib: The Essential Manual For Every Patient With Atrial Fibrillation
Technical Issues With Pulmonary Vein Isolation
Let’s first talk about areas of the heart tissue growing back after an ablation. Now, universally for most people’s atrial fibrillation, the main target for ablation is an area called the pulmonary veins, which is located in the left atrium, or left upper chamber of the heart. The pulmonary veins are where most people’s AFib comes from, and this is the most common area in the heart that triggers episodes of atrial fibrillation. If you’d like to know more about what happens during a catheter ablation for atrial fibrillation, including pulmonary vein isolation,check out my article about the AFib ablation procedure details. But as far as the procedure itself, targeting and ablating the areas around the pulmonary veins in order to block the short circuit signals that trigger episodes of AFib, is the most common goal for an AFib ablation.
However, in past clinical studies when they have looked at people who have had recurrences of AFib, meaning AFib that comes back after ablation, in those settings where the patients end up getting another ablation procedure, a common thing that is found is that pulmonary veins have reconnected or the heart tissue has grown back. So why would a pulmonary vein reconnect after it’s already been ablated? Well, the heart can be amazingly resilient, and even though during an ablation procedure, it’s the electrophysiologist’s goal to actually to intentionally burn or create scar areas of the heart in order to reduce AFib. The heart can be amazingly resilient and actually grow back, and there’s a few reasons that that can happen.
During an ablation procedure, the electrophysiologist can see if the normal heart signals that he’s trying to ablate have been successfully ablated, and that’s fairly simple to see an ablation catheter. However, what might be happening is that the tissue that is trying to be ablated is not thoroughly and completely ablated, it may just be stunned or swollen to where it hasn’t been completely ablated. Then over time, usually over a period of several weeks, that swelling subsides and then the tissue reconnects and goes back to normal, this is the main way that sometimes heart tissue can grow back.
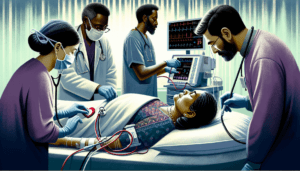
Now over the years, the technology that is used during an ablation, in order to have more thorough ablation lesions, and to prevent the areas from coming back is always continuing to improve and change. I frequently mention to my patients that the equipment to do ablation procedures, changes every year like an iPhone does, there’s always new models and new versions of equipment that are coming out in order to try to improve the success rate. Most importantly, over the last few years, several of the ablation catheters now have what is called contact sensing. It basically gives a feedback to the doctor to know how strong the catheter is touching the heart. You can imagine how difficult it can be to get good contact with a beating heart while you’re trying to do a procedure on someone, and so these sensors have allowed doctors to get better contact with the heart tissue, as well as hopefully provide more thorough ablation lesions.
A second reason for technical failure is, I would say is a “knowledge deficit.” This is more important for people who are in more advanced stages of atrial fibrillation. As I have mentioned in the past, AFib is a disease that progresses over time, if you want to learn more about stages of AFib, check my article on the progression of AFib. Atrial fibrillation is a disease that progresses, it inherently changes the microscopic features inside of the heart and inside of the left atrium where AFib usually comes from. As people get more and more episodes of atrial fibrillation, especially people who are in an AFib all the time or most of the time, there tends to be a lot of scar tissue, or fibrosis, inside of the left atrium. As a result, as people develop more advanced stages of atrial fibrillation, the routine ablation, which involves only ablating around the pulmonary veins, may not be sufficient enough just because the heart has changed so much after all the episodes of AFib and all the duration of a patient’s AFib
Many times in patients with more advanced AFib, an ablation procedure will frequently require an ablation that is more than just the pulmonary veins in order to get a better success rate. However, what defines that “more ablation is needed” is something that does not have a clear consensus about what to do at this time. There have been many research studies over the years about strategies on how to ablate people who are in more advanced stages of AFib, and unfortunately all the research results don’t give any clear consensus. That is why the strategy to ablate someone’s AFib who was in more advanced stages of AFib, is pretty much based on what your doctor’s preferences are, as well as your doctors past experience. But there is no clear standard definition that says all doctors or all electrophysiologists should ablate this amount or not this amount when someone is in more advanced stages of a AFib. Despite many past research studies, there has been no clear consensus. AFib changes people’s hearts very differently, and one heart is different than another, which is in my opinion, part of the reason why there’s been no clear consensus.
In my opinion, what’s going to give people with more advanced stages of AFib better results is going to be to customize their AFib ablation, meaning having a good strategy to most determine what, in an individual patient, are the areas that need to be ablated. This is easier said than done, again, there have been many research studies which have clearly not giving an answer to this question at this point. Some of the past clinical studies involve very complex mathematical models to try to figure out what in each individual patient is causing each individual patient’s AFib. But again, still no clear consensus, but I am convinced that someday there will be a clear, simple, straightforward way for any electrophysiologist to figure out what are the most necessary areas to ablate for a person with advanced AFib to improve their success rate, in a customized fashion.
How Else Can I Improve The Success Rate of An AFib Ablation?
Another reason why some people exeprience AFib after an ablation is what I would call: “missing pieces of the puzzle.” There are many factors that are outside of the ablation itself which have been found to improve the success rate of the ablation procedure as well. Most of these are involved in the category of lifestyle modifications or managing other health conditions. Probably one of the most studied lifestyle modification that can also improve AFib ablation is weight loss. Weight loss had been found to significantly improve AFib, but it has also been found to improve AFib in the setting of a catheter ablation, to improve the success rate of the ablation itself.
When patients are overweight they are also at increased risk for high blood pressure and diabetes, which can also contribute AFib, as well as increasing the scar tissue in the left atrium. However, the fat molecules themselves, whether that’s fat molecules around the waist or even fat molecules that develop around the heart tissue, can all secrete hormones which increase inflammation, which can then in turn continue to lead to progressions of AFib. That is a reason why weight loss has been shown to have significant improvement in AFib. And one of the biggest diet studies to date called the LEGACY trial.
During the LEGACY trial, patients who got an ablation procedure and lost weight, ideally over 10% of the initial starting weight, had the highest success rates from the ablation procedure, versus people who got an ablation procedure but did not lose any weight or did not change their lifestyle, did not have a very good success rate. This can be a clue in terms of why doesn’t a procedure work sometimes, that more things need to be done than just the ablation procedure itself. Clearly an ablation procedure combined with the right lifestyle modifications can make a dramatic and significant improvement in person’s AFib, as well as improving the success rate of the procedure itself.
Another topic that has been shown to have significant improvement AFib as well as having a significant improvement in the success rate of an ablation procedure, is management of sleep apnea. Sleep apnea also happens to be strongly correlated with obesity. In sleep apnea, patients frequently stopping breathing while they are asleep, and that can happen many times and there has been a very clear association with sleep apnea with atrial fibrillation, as well as improving the success rate of an ablation procedure with sleep apnea treatment. There’ve been studies that have clearly shown that if someone has an ablation procedure and also is properly being treated for sleep apnea, if they have it, then that person is going to have a higher success rate from the ablation procedure as well. If you’d like to read more about sleep apnea and how it affects AFib, check out my article on sleep apnea and atrial fibrillation.
Weight loss and sleep apnea are probably the most commonly studied, in terms of lifestyle modifications or other health conditions where that improving those health conditions can also make a significant improvement in someone’s AFib, as well as improving the success rate of an AFib ablation procedure. But there are also other health conditions which can also show improvement which include strict management of high blood pressure, diabetes, also evaluation and need for any treatment for thyroid related disorders just to name a few. But I would discuss with your doctor which additional lifestyle modifications may be needed for you.
So what tips can I give to someone who continues to experience AFib even after an ablation procedure? In my opinion, it would be best to start off with the lifestyle modifications such as those listed above first, weight loss or treating sleep apnea may make a huge difference in improving AFIb symptoms. Many patients get multiple ablation procedures performed because an underlying health condition is not properly treated. If none of these lifestyle medications apply to you, sometimes additional ablation procedures will be needed. Always discuss with your doctor which treatment options are right for you.
Hopefully this article can be helpful for you if you’ve had an ablation procedure and still struggle with symptoms of AFib, please discuss with your doctor what are the right treatment options for you. In addition, if you’re looking for an online program to help you with implementing these lifestyle modifications to your life and improving the success rate from any ablation procedures, check out my program, Take Control Over AFib.
The Best Atrial Fibrillation Book
Your Complete Guide To AFib: The Essential Manual For Every Patient With Atrial Fibrillation

Shop AFib Products on Amazon
KardiaMobile 6-Lead Personal EKG Monitor – Six Views of The Heart – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Works with Most Smartphones - FSA/HSA Eligible
13% Off
KardiaMobile 1-Lead Personal EKG Monitor – Record EKGs at Home – Detects AFib and Irregular Arrhythmias – Instant Results in 30 Seconds – Easy to Use – Works with Most Smartphones - FSA/HSA Eligible
$79.00 (as of June 16, 2025 15:14 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display
(as of June 16, 2025 08:46 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Fitbit Sense 2 Advanced Health and Fitness Smartwatch with Tools to Manage Stress and Sleep, ECG App, SpO2, 24/7 Heart Rate and GPS, Shadow Grey/Graphite, One Size (S & L Bands Included)
10% Off
OMRON 2-in-1 Upper Arm Blood Pressure Monitor & 1-Lead EKG Monitor - Clinically Validated Blood Pressure Arm Cuff & Machine - Use OMRON Connect App
24% Off
Samsung Galaxy Watch 6 44mm Bluetooth Smartwatch, Fitness Tracker, Personalized HR Zones, Advanced Sleep Coaching, Heart Monitor, BIA Sensor, Health Wellness Insights, Big Screen, US Version, Graphite
$353.21 (as of June 16, 2025 07:34 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Natural Rhythm Triple Calm Magnesium 150 mg - 120 Capsules – Magnesium Complex Compound Supplement with Magnesium Glycinate, Malate, and Taurate. Calming Blend for Promoting Rest and Relaxation.
$20.77 ($0.17 / Count) (as of June 16, 2025 07:34 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
Pure Encapsulations Magnesium (Glycinate) - Supplement to Support Stress Relief, Sleep, Heart Health, Nerves, Muscles, and Metabolism* - with Magnesium Glycinate - 180 Capsules
$44.60 ($0.25 / Count) (as of June 16, 2025 08:46 GMT -06:00 - More infoProduct prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.)
















![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #1](https://m.media-amazon.com/images/I/311xwtp4mFL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #2](https://m.media-amazon.com/images/I/41j+8AaUGsL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #3](https://m.media-amazon.com/images/I/41jIyxZitnL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #4](https://m.media-amazon.com/images/I/41IpNJERjCL._SL100_.jpg)
![Apple Watch Series 9 [GPS 41mm] Smartwatch with Storm Blue Aluminum Case with Silver Sport Band M/L. Fitness Tracker, Blood Oxygen & ECG Apps, Always-On Retina Display #5](https://m.media-amazon.com/images/I/31o17yhfYpL._SL100_.jpg)